Department News
On May 4th, 2025 the Provincial Department of Anesthesiology hosted the 37th Annual Anesthesiology Resident Research Day.
Award Recipients
Congratulations to all award recipients for their exceptional contributions to our department.
Research Competition Awards:
- Dr. William McKay RESIDENT RESEARCH AWARD “Best Completed Project” ($500) - Sarah Larmour
- Best In Progress Project ($200) - Anulika Nwakaeze
- Best Study Design ($200) - Seb Turcotte
- Best Presentation ($100) - Allan Meldrum
- Best Poster ($100) - James Macaskill
Provincial Department of Anesthesiology Environmentally Sustainable Health Systems Award:
Dr. Allison Crichlow (Regina, Sk)
About the Award:
The primary purpose of this Award is to recognize a department member for their resourcefulness, leadership, and dedication to environmentally sustainable health systems. An environmentally sustainable health system is one that improves, maintains, or restores health while minimizing negative impacts on the environment and leveraging opportunities to restore and improve it, to the benefit of the health and well-being of current and future generations.
This prestigious recognition is a testament to Dr. Crichlow's unwavering commitment to sustainability and environmental responsibility in our healthcare system. She is specifically recognized for her groundbreaking efforts to reduce waste in the operating room. Her innovative actions have not only led to significant improvements in facility sustainability but have also inspired colleagues to adopt more environmentally conscious practices.
In appreciation of her exceptional efforts, she was formally recognized at the Anesthesiology Resident Research Day event and was provided with a monetary prize of $2,000. This honor symbolizes our esteem and appreciation for Dr. Crichlow's significant contributions to fostering a culture of sustainability within our organization.
SK CAS Essay Contest Winners:
- 1st Place: Kevin Jun Won Lee, University of Saskatchewan, College of Medicine
"The Ace of All Trades in Medical Research – The Impact of an Academic Anesthesiologist" Link - 2nd Place: Mackenzie Heidel, University of Saskatchewan, College of Medicine
"Social Prescribing: A Perioperative Strategy for Humanistic Anesthesia" Link
Feedback
Your thoughts and feedback on the event are important to us. Please take a few minutes to complete the post-event survey. Your responses will remain anonymous and confidential, and we will consider your feedback for future events
Feedback Survey Link
Event Resources
The Abstract Booklet  can be viewed here: Link
can be viewed here: Link
Research Posters:
-
Ava Bayat “Co-developing a Multidisciplinary Delirium Prevention Pathway to Reduce Postoperative Delirium in Older Adults with Cognitive Frailty” Link
-
Aishwarya Gannamani “Indications for Issuing Difficult Airway Alerts in Anesthesia in Saskatchewan” Link
-
Melissa Herdzik “Ocular Radiation Exposure Among Anesthesiology Staff and Residents: Are We Exceeding the Occupational Limits?” Link
-
Nigel Hey “Implementing Cadence: Assessing the feasibility of long-term follow up in ICU bereavement” Link
-
Muxue Li “Optimizing Fasting Duration in Older Malnourished Orthopedic Fracture Patients: A Study of Current Practices in Regina” Link
-
James Macaskill “Cardio-Cerebral Coupling and Rectal Oxygenation: A Physiologic Study in Anesthetized Pigs” Link
-
Hifsa Noor “Assessing Stomach Fullness with Gastric Ultrasound in surgical patients who are taking GLP-1 agonists pre-operatively” Link
-
Olivia Woo “Effectiveness of Infographics in Translating and Retaining Anesthesia Knowledge Among Clerkship Medical Students” Link
-
Jenil Patel (Honours Student) “Investigating the Support Needs of Family Physician Anesthetists in Saskatchewan, Canada” Link
Family Practice Anesthesiologist Presentation:
- Kiranjot Bhangoo "Exploring a Team-Based Model of Anesthesia Care in Saskatchewan; Understanding Options and Assessing the Potential for Change" Supervised by Dr. Mateen Raazi Link
Photos

Check out The Wake Up [Research Edition] for more on this event and the research taking place in the Provincial Department of Anesthesiology:Link

About Us
Welcome to the Provincial Department of Anesthesiology, an academic and clinical department within the College of Medicine (CoM), University of Saskatchewan, and the Saskatchewan Health Authority (SHA). With the introduction of a single health authority in Saskatchewan on Dec 04, 2017, our department continues to grow as a cohesive group of over 150 members. This includes 130 Specialist anesthesiologists (115 CoM faculty members), 26 Family Practice Anesthetists and affiliated.
The members of our department are fully engaged as clinicians, physician leaders, academics, educators and researchers throughout the Province. We provide safe and high quality connected clinical care, innovative education and cutting edge research benefiting the people of Saskatchewan and beyond. Our members provide clinical and other services in a variety of locations including hospital and non-hospital facility operating rooms, pre-operative assessment clinics, maternal and child care units, critical care units and other areas.
We, the faculty, residents, and staff of the department invite you to learn more about what anesthesiology can offer to you as a learner, interested colleague and current or future patient.
Be well,
Dr. Mateen Raazi, MD, FRCPC
Provincial Department Head Anesthesiology
Provincial Department of Anesthesiology
University of Saskatchewan
The Provincial Department of Anesthesiology Podcast: Airway Breathing Conversation
Are you ready to learn your ABC's? Run by Anesthesiology residents at the University of Saskatchewan, this podcast was created with the goal of providing individuals with anesthesiology-related medical information. Created/hosted by Dr. Alixe Pellerin (Anesthesiology PGY3) and produced/edited by Dr. Allan Meldrum (Anesthesiology PGY1), join us twice a month while we speak with co-residents, anesthesiology staff, members of the broader USask College of Medicine Community, and other special guests about all things anesthesia.
The ABC Podcast is excited to cover a wide variety of anesthesia-related topics, including life as an anesthesiologist, research here in Saskatchewan, how anesthesia has changed over the past few decades, how other healthcare professionals see anesthesia, residency/CaRMS information, quick education bites/technical tips, and much, much more!
Whether you are an anesthesiologist, resident, medical student, or member of the general public, join us as we demystify the incredible specialty that is anesthesiology!
Podcast & social media links available at: http://linktr.ee/abc_podcast
___________________________________________________________________________________
Anesthesiology Social Media Hub
The USask Provincial Department of Anesthesiology is committed to engaging with the public and demystifying anesthesia's role in caring for patients both inside and outside the operating room. That's why we've created a new "hub" with all of our community engagement links in one place, helping to make it even easier to access our many projects and social media accounts!
Be sure to check out the many links already available: Our social media accounts, the Department's YouTube channel, Our resident-run podcast: "Airway, Breathing, Conversation", and so much more!
Be sure to bookmark this link to stay up-to-date: https://linktr.ee/usask_anesthesia.
Message from the Director of Quality Improvement and Safety
The Provincial Department of Anesthesiology strongly believes in continuous quality improvement and patient safety. We are pioneers in establishing a departmental Quality Assurance Committee focusing on real life case review scenarios to determine how healthcare systems need to change to improve patient care in Saskatchewan. Dr. Richard Schaan leads this incredible team, communicating the committee’s findings to foster meaningful positive change. Quality improvement and patient safety is innate in the work anesthesiologists in our department do every day as we strive to provide the best anesthesia care possible.
We welcome patients, families, healthcare professionals, and fellow colleagues to share their ideas and stories so that we can continue to improve healthcare in Saskatchewan. Please contact Dr. Vicky Loessin (vicky.loessin@saskhealthauthority.ca) with any thoughts or ideas.
Dr. Vicky LoessinDirector of Quality Improvement and Safety
Provincial Department of Anesthesiology
University of Saskatchewan
__________________________________________________________________________________
Message from the Quality, Safety & Continuous Improvement Facilitator
One of my favourite stories about change was told by Dr. Atul Gawande, a surgeon, called “Slow Ideas”. In it, Dr. Gawande talks about the different trajectories of surgical anesthesia and antiseptics, both of which were discovered in the 19th century. He tells the story better than I ever could so check it out here: Link.
What I like about this story is what we can learn from it – about how we can make changes happen more quickly, systematically, and effectively. Changes not for change’s sake but actual improvements that make a difference in peoples’ lives and experiences. This is at the heart of quality improvement – making good change and working towards “better”.
I already see how highly valued safety, quality, and good care are in the Provincial Department of Anesthesiology. I hope to be able to contribute what I can to your efforts. I would love to talk about any ideas for improvements you have, please reach out anytime!
Carla FloganQuality, Safety & Continuous Improvement Facilitator
Provincial Department of Anesthesiology
University of Saskatchewan
carla.flogan@usask.ca
Strategic Plan
Provincial Department of Anesthesiology Strategic Plan
Vision, Mission, and Strategic Priorities
We have developed our vision, mission, and strategic priorities as follows:
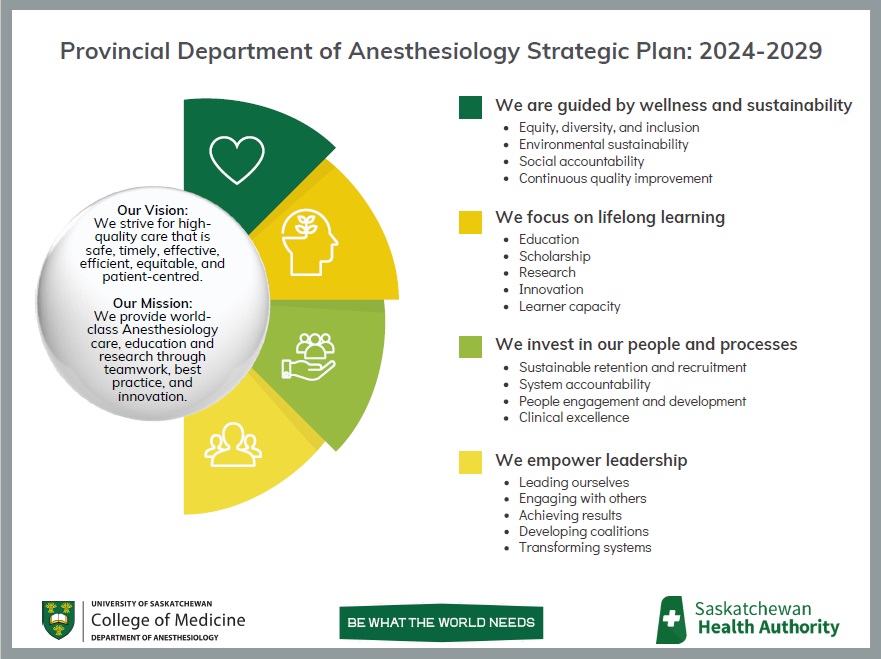
We are continuously working towards these aspirations through our ongoing projects and tasks. If you have any questions about our plan, please contact Anesthesia.Mailbox@saskhealthauthority.ca.
News
Saskatchewan Centre for Patient-Oriented Research (SCPOR) and The University of Saskatchewan, College of Medicine-PGME:
James Macaskill. SCPOR Traineeship Funding. Harnessing the Value of an Electronic Medical Record in Implementing Virtual Pre-Surgery Assessments Across Saskatchewan. ($10,000) May 7th, 2025.
Nigel Hey. SCPOR Traineeship Funding. Evaluating Saskatchewan’s First ICU Bereavement Program. ($10,000) May 7th, 2025.
37th Annual Anesthesiology Resident Research Day:
Research Competition Awards:- Dr. William McKay RESIDENT RESEARCH AWARD “Best Completed Project” ($500) - Sarah Larmour
- Best In Progress Project ($200) - Anulika Nwakaeze
- Best Study Design ($200) - Seb Turcotte
- Best Presentation ($100) - Allan Meldrum
- Best Poster ($100) - James Macaskill
Provincial Department of Anesthesiology Environmentally Sustainable Health Systems Award: Dr. Allison Crichlow, Anesthesiologist, Regina, Sk
Saskatchewan Health Research Foundation (SHRF):
Dr. Mateen Raazi, Dr. Lei Xia, Dr. Jennifer O’Brien, Dr. Rhonda Zwack, Heather Dyck, Diana Ermel, Candace Abramyk, & Carla Flogan. Anesthesia Health Human Resource Solutions for Saskatchewan: A Knowledge Mobilization Study. Saskatchewan Health Research Foundation’s (SHRF) 2024-25 Mobilize Grant Call #2. ($9,927.84)
USask College of Medicine
Congratulations to Dr. Ryan Pikaluk for being selected for the College of Medicine Regina Campus Teaching Award, 2025. The award will be presented at the Regina College of Medicine Appreciation Night on May 15th, 2025.
Congratulations to Dr. Justina Koshinsky for being selected for the College of Medicine Faculty Leadership Excellence Award, 2025. The award will be presented at the College of Medicine Appreciation Event on May 21st, 2025.
Provincial Department of Anesthesiology Research Engagement & Excellence (DARE) Awards
Research Engagement Awards:
Drs Jonathan Gamble and James Macaskill. Cardio-cerebral Coupling: An Experimental Study of Cardiac Output and Cerebral Blood Flow in Porcine Models. Awarded $5,000.
Drs Michelle Clunie, Oksana Prokopchuk-Gauk, and Devin Edwards. A Survey of Acute Normovolemic Hemodilution Use in Canada. Awarded $1,700
Research Excellence Award:
Dr. Jonathan Gamble. A Prospective Randomized Controlled Trial of Electroconvulsive Therapy with Ketamine Anesthesia (Standard Therapy) and High Intensity Ketamine with Electroconvulsive Therapy Rescue for Treatment-Resistant Depression – EAST HIKER Trial. Awarded $13,000
Saskatchewan Health Research Foundation (SHRF):
Raazi M, O’Brien J, Flogan C, Abramyk C, Ermel D, Dyck H, Bhangoo K, Sivertson J, Earle D, Khan M. Exploring a Team-based Model of Anesthesia Care in Saskatchewan; Understanding Options and Assessing the Potential for Change. 2024-2025 Saskatchewan Health Research Foundation’s (SHRF) Align Grant Call #3 ($9,924)
Heather Dyck, Patient Partner. Recognizing SHRF Connections Award. 21st Annual Santé Awards. January 30th, 2025
2025 COM Dean's Summer Research Project Awardees:
Dr. Jonathan Gamble. Repeat Neuroimaging in Children with Epilepsy, Autism Spectrum Disorder, Global Developmental Delay, and Cerebral Palsy Under General Anesthesia: A study to investigate Rate of New Significant Neuroimaging Abnormalities, Adverse Anesthesia Events, and Family Experience
Dr. Peter Hedlin. Can bispectral index be used as a rapid tool for measuring patient cognition and frailty before surgery
Saskatchewan Centre for Patient-Oriented Research (SCPOR)-College of Medicine:
Dr. Ava Bayat, Co-developing, Implementing, and Evaluating a Multidisciplinary Delirium Prevention Pathway to Reduce Postoperative Delirium in Older Adults. SCPOR-PGME Traineeship Funding. Supervised by Dr. Peter Hedlin ($10,000) November 14th, 2024.
2024 PGME Resident Research Day:
Allan Meldrum: Second Place, SCPOR Trainee. The Misunderstood Anesthesiologist: A Prospective Cohort Study Comparing the Effectiveness of Educational Media in Preoperative Assessment Clinics. Supervised by Dr. Henry Bi
Trevor Krysak: Second Place, Resident Research Presentation. Safety of a Catheter-Over-Needle (CON) System for Epidural Placement in a Porcine in vivo Model. Supervised by Dr. Jon Gamble
Alison Knapp: Third Place, Resident Research Presentation. Intensive End of Life Care: Implementation of a Guideline-Based Order Set for the Withdrawal of Life-Sustaining Therapy in the Intensive Care Unit in Saskatoon Health Region. Supervised by Dr. Sabira Valiani
Saskatchewan Health Research Foundation (SHRF):
Dr. Gaurav Jain, Dr. Trevor Krysak, Dr. Jennifer O’Brien, Darcie Earle, Jess Klaassen-Wright, & Maria Cruz. Saskatchewan Health Research Foundation’s (SHRF) 2024-25 Align Grant Call #1.The Perioperative Experience of Patients Undergoing Gender Affirmation Surgery in Saskatchewan. ($9,990.06)
Peter Hedlin, Dr. Jennifer O’Brien, Dr. Megan Surkan, Dr. Nathan Ginther, Ms. Ronda Wedhorn, Mrs. Heather Dyck, Dr. Lilian Thorpe, Dr. Huma Aftab, & Dr. Liam Dowling. Co-developing, Implementing, and Evaluating a Multidisciplinary Delirium Prevention Pathway to Reduce Postoperative Delirium in Older Adults with Cognitive Decline: A Pilot Study. 2023-24 SHRF Solutions-Innovation Grant in partnership with Alzheimer Society of Saskatchewan ($49,641.21).
Canadian Society for Clinical Investigation/Canadian Institutes of Health Research
Congratulations to anesthesia resident Dr. Alison Knapp for being chosen as a successful recipient of the 2024 CSCI/CIHR Resident Research Award for the College of Medicine, University of Saskatchewan. This prize is awarded annually for the best resident research project conducted during a RCPSC/CFPC training program at each Canadian medical school. The prize for this award includes $1,000.00, a complimentary CSCI membership for 2 years, and a certificate signed by the CIHR & CSCI presidents. Alison will be recognized at PGME's Celebration Night and awards ceremony in Saskatoon on Friday November 22nd, 2024. Learn more about the award.
Canadian Anesthesiologists' Society (CAS)
Congratulations to medical student Noaah Reaume for receiving the award for Best Abstract in Obstetric Anesthesia at the 2024 CAS meeting in Victoria, June 7-10, 2024. The winning abstract titled The Incidence of Spinal Anesthesia Failures During Elective Caesarean Sections: A Comparison of Two Different Suppliers, was supervised by Dr. Peter Hedlin.
University of Saskatchewan Retirees Association (USRA)
Congratulations to Dr. Bill McKay for receiving the Continuing Contribution Award from the University of Saskatchewan Retirees Association. Dr. McKay was formally recognized at the awards dinner held on Thursday, May 31st, 2024.
College of Medicine
Congratulations to Dr. Jennifer O'Brien for being chosen as the recipient of a College of Medicine Strategic Star Award in the priority category of Strengthening Research Capacity. This award recognizes staff members whose exceptional actions have contributed to one of the COM Strategic Priorities. Dr. O'Brien will be presented with her award at the upcoming COM Recognition Event on Thursday June 13th.
Faculty Profiles
Undergraduate Program
The Provincial Department of Anesthesiology has significant involvement in the undergraduate MD program.
Members are involved with pre-clinical teaching on local anesthesia pharmacology, general anesthesia pharmacology and perioperative medicine. In addition, many of our faculty participate in small group clinical skills teaching, communications skills sessions, simulation and OSCE examinations.
We have a popular shadowing program for first- and second-year USask medical students looking to explore the specialty and a vibrant student-led Anesthesia Interest Group. Students can also compete in our annual essay competition, the Bev Leech Anesthesia Book Prize.
USask third year clerks complete a core two-week anesthesiology rotation in either Saskatoon, Regina or Prince Albert. The overall objective of this rotation is to provide students with the skills and knowledge that is both practical and generalizable to the primary care physician.
The Department also offers elective anesthesia rotations to clerks from USask, other medical schools in Canada and approved international schools.
Elective students can expect to gain further generalist experience in the provision of anesthetic care in a wide compliment of general and subspecialty surgical services which may include:
- Pediatric
- Obstetric
- Vascular
- Neuro
- Thoracic
- Acute pain
- Regional
- Chronic pain
- and Trauma
We do not offer clerk electives exclusively in any individual subspecialty. Please contact the departmental staff should you have any questions!
Dr. Melanie Orvold
Director of Undergraduate Anesthesiology Education
Provincial Department of Anesthesiology
University of Saskatchewan
Dr. Melanie Orvold
Director of Undergraduate Anesthesiology Education & Saskatoon Clerkship Core Rotation Director
Dr. Mofolashade Onaolapo
Education Director, Regina Site
Dr. Derrick Williams
Education Director, Prince Albert Site
Shumaila Zafar
Administrative Assistant, Saskatoon Site
Trisha DeMars
Administrative Assistant, Regina Site
306-766-3771
Nicole Toutant
Administrative Assistant, Prince Albert Site
Postgraduate Program
Welcome to the University of Saskatchewan Anesthesiology Residency Program!
The USask Anesthesiology program is a five-year training program based out of Saskatoon, the largest city in Saskatchewan. Residents have opportunities for training opportunities in Regina the Province’s capital, Prince Albert as well as partnerships with chronic pain in Calgary, AB.
Our competence by design-based training program is supported by weekly academic half-days, weekly case rounds, as well as a longitudinal simulation and POCUS program. Faculty come from diverse backgrounds and bring fellowship training from all areas of subspecialty anesthesia to their practice and are eager to teach and share their knowledge.
We have a very productive research team led [1] by Dr. Jon Gamble and supported by Research Associate Dr. Jennifer O’Brien, Provincial Research Facilitator Darcie Earle, Statistician Dr. Mary-Ellen Walker, Clinician Scientist Dr. Peter Hedlin, as well as partnerships with the College of Veterinary Medicine.
Our program has pioneered a number of initiatives – including a robust wellness program[2], one of the first longitudinal POCUS curriculums in anesthesiology[3] and most recently a Quality assurance curriculum.
Our residents are well-respected as some of the strongest clinicians as well as kindest colleagues. After residency, our residents go on to pursue fellowships of their choice both nationally and internationally or go straight into independent practice with the confidence to be a well-rounded anesthesiologist.
Dr. Eugene Choo
Program Director
Provincial Department of Anesthesiology
University of Saskatchewan
[1] https://medicine.usask.ca/department/clinical/anesthesiology.php#Research
[2] Chakravarti A, Raazi M, O'Brien J, Balaton B. Anesthesiology Resident Wellness Program at the University of Saskatchewan: curriculum content and delivery. Can J Anaesth. 2017 Feb;64(2):199-210. English. https://doi: 10.1007/s12630-016-0773-0. Epub 2016 Nov 14. PMID: 27844198.
[3] Clunie, M., O’Brien, J., Olszynski, P. et al. Competence of anesthesiology residents following a longitudinal point-of-care ultrasound curriculum. Can J Anesth/J Can Anesth (2021). https://doi.org/10.1007/s12630-021-02172-2
Welcome to the Postgraduate Anesthesia Program at the University of Saskatchewan!
Our fully Royal College accredited, five-year postgraduate training program provides comprehensive training in anesthesiology, based in Saskatoon, Saskatchewan, with a distributed program in our province's capital, Regina. Residents gain broad exposure to both generalist and subspecialty anesthesia, ensuring a well-rounded experience across diverse clinical settings within the province including a multidisciplinary chronic pain clinic in Regina.
Our program follows a Competence by Design framework, supported by a strong academic curriculum featuring weekly dedicated academic half-days, one of the most comprehensive simulation and point-of-care ultrasound (POCUS) programs in the country, and a focus on innovation in medical education. We have pioneered several key initiatives, including a robust wellness program, one of the first longitudinal POCUS curriculums in anesthesiology and a newly developed quality assurance curriculum.
Graduates from our program successfully pursue subspecialty fellowships across Canada and internationally or enter independent practice as confident, well-rounded generalists. Whether your goal is fellowship training or a strong foundation for generalist practice, the University of Saskatchewan provides the training and support to help you succeed.
Whether you are a medical student interested in post-graduate training or a resident exploring elective opportunities, we invite you to explore our program and discover what makes anesthesia training at the University of Saskatchewan unique!
For more information, please visit the CaRMS website.
Dr. Eugene Choo
Program Director
Dr. Calvin Lo
Assistant Program Director
Dr. Jessica Bruce
Assistant Program Director - Curriculum
Megan Fortosky
Program Administrator, Undergraduate
& Postgraduate Education, Saskatoon Site
306-655-1193
Chelsea Malkowich
PGME Program Administrator, Saskatoon Site
306-966-6148
Dr. Ryan Pikaluk
Education Site Director - Regina Site
Dr. Joelle McBain
Assistant Education Site Director - Regina Site
Continuing Education and Professional Development Events
The Provincial Department of Anesthesiology holds weekly grand rounds at 07:00-08:15 AM on Fridays at Health Science E1130. These are Royal College CME accredited events. The speakers range from residents to staff anesthesiologists. We often have multi-disciplinary sessions. If you have any questions please email: Henrybi@gmail.com
If you have an idea for Grand Rounds, please complete the Grand Rounds Idea Form to populate the Grand Rounds Idea Repository.
Dr. Henry Bi
Director of Continuing Education and Professional Development
Provincial Department of Anesthesiology
University of Saskatchewan

The SASK-PULSE (Saskatchewan Anesthesia Skills & Knowledge: Practical, Up-to-date Learning, Simulation & Education) Workshop held on Saturday, April 5, 2025, in the CLRC (Clinical Resource Learning Center) at the Health Sciences Building in Saskatoon was a resounding success! The event brought together Family Practice Anesthesiologists and FRCPC Specialist Anesthesiologists from across the province for a day of practical, hands-on learning focused on PoCUS (Point of Care Ultrasound) and ultrasound-guided vascular access.
Participants benefited from expert instruction, valuable simulation experiences, and dedicated time to refine key clinical skills. Just as importantly, the workshop fostered meaningful networking opportunities, helping to strengthen the connections among Anesthesia practitioners across Saskatchewan.
Thank you to everyone who contributed to making this event a success, and a special thanks to Dr. Justina Koshinsky and the entire SASK-PULSE team for their leadership and coordination. As well as the continued support from the Saskatchewan Medical Association, which made this day possible. We look forward to building on this momentum with future CME events.

_________________________________________________________________________
Amazing Race: AIRWAY
On April 7, 2025, anesthesia residents took on the first-ever Amazing Race: AIRWAY—a high-energy, low-stakes, team-based competition designed to boost airway knowledge and skills through a gamified, hands-on format.
Seven Pit-stops, riddles, timers, crisis communication, team spirit, and laughter.
Residents worked in small teams, racing against the clock to solve airway challenges, decode clues, and practice vital technical and non-technical skills.
This unique learning opportunity wouldn’t have been possible without the incredible efforts of Dr. Justina Koshinsky, the Simulation Team, and the CLRC staff, whose creativity, organization, and enthusiasm made it a standout success.
Objectives met:
- Reinforced airway knowledge and hands-on skills
- Practiced team-based problem solving and crisis communication
- Strengthened camaraderie within the residency group
It was an unforgettable day of learning, teamwork, and fun. Congratulations to all the residents who participated, especially the top-scoring teams, who earned well-deserved bragging rights. We can’t wait to see what’s in store for next year!

The Anesthesiology Journal Club provides faculty and residents a valuable opportunity to present their own research and to present on recent publications relevant to the area of Anesthesiology. This forum offers residents the chance to enhance their critical appraisal and public communication skills. Residents will explain the rationale and methodology of their own project for peer-review and lead an evidence-based discussion of selected publications.
The Journal Club meets at 17:30 on the third Thursday of every month from September to April. Each meeting features a minimum of one original research presentation, and one critical appraisal of a journal article and related discussion. The Department of Anesthesiology’s research staff, faculty, residents and collaborators are invited to attend the meetings.
Articles are chosen by the resident and links to the articles are circulated one week prior to the meeting.
If you have a Journal Club idea, please complete the Journal Club Ideas Form to populate the Journal Club Ideas Repository.
If you are interested in learning more about Journal Club or attending as a guest, please contact Darcie Earle, Provincial Research Facilitator.
Scholarly Activity
Welcome to the University of Saskatchewan Provincial Department of Anesthesiology Research Program.
With support from the College of Medicine and the Provincial Department of Anesthesiology, we strive to advance the science of our discipline. We embrace the University of Saskatchewan’s culture of collaboration and diligence to pursue research excellence. Our goals are to produce high impact knowledge recognized and celebrated locally, regionally, nationally, and internationally.
With the efforts of our dedicated faculty, students, residents and staff, the Research Division conducts a broad range of research - from the bench to the bedside. These efforts include:
- Postoperative Cognitive Dysfunction
- Medical Education
- Perioperative Fasting
- Resuscitation
- Airway Assessment
- Mood Disorders
- Virtual Care
While I am privileged to lead the Research program, we are fortunate to have a highly skilled and dedicated research team. Our team includes: Dr. Peter Hedlin (Clinician Scientist), Dr. Jennifer O’Brien (Research Associate), Darcie Earle (Provincial Research Facilitator), and Dr. Mary Ellen Walker (Statistician).
We have recently launched a provincial research and innovation funding program - Provincial Department of Anesthesiology Research Excellence and Engagement Awards (DARE-Awards). For program details feel free to contact myself or Darcie Earle, Provinicial Research Facilitator.
If you are interested in learning more about our research endeavors, feel free to contact us directly. We always invite collaboration from the broad scientific community to add to the breadth and impact of Anesthesiology research.
Dr. Jonathan Gamble, MD, FRCPC (Anes, Crit Care)
Executive Director of Research
Provincial Department of Anesthesiology
University of Saskatchewan
Welcome to the Provincial Department of Anesthesiology webpage and our Research Program.
I had the privilege of joining the department in 2018 in both a clinical and research capacity. During my time here I’ve been incredibly impressed by the collaborative and supportive nature of our research members and support staff.
Being in the early stages of my career, one of the initial challenges has been to develop an area of research focus. There are so many fascinating areas of research in the world of anesthesia and perioperative medicine, it’s hard to narrow the list down.
In our Department, we have ongoing research in multiple and diverse areas of Anesthesiology including Cardiac Anesthesia, Medical Education, Social Equity, and Physician Wellness. My areas of research include Quality Improvement, Cardiac Anesthesia, and in particular, Perioperative Care.
My perioperative care research program builds upon my pre-medicine interests and research activity related to developing a vaccine for prion diseases. Prions are transmissible misfolded proteins that can cause rapidly progressive cognitive decline and death in the affected individual. Still fascinated by neuroscience, I became interested in the cognitive changes that occur in the perioperative period. More and more evidence suggests that certain populations of patients are at high risk for developing cognitive dysfunction following surgery. In most cases, the effects are temporary, but for some patients it can be a long lasting, or even permanent change. The cognitive decline can end up affecting a patient’s length of hospital stay, and the level of care required once they are discharged. At this point we still don’t have a good understanding of what causes it, or how we can prevent it.
Our research program continues to grow. I am currently focused on establishing collaborations with other centres in Canada who are already working in the area of post-operative cognitive dysfunction. Our department is currently participating in a multicentre trial looking at the effects of benzodiazepines on delirium following cardiac surgery. Next steps for our research program include expanding our research support team so that we can continue our current projects while fostering the increased demand for participation in valuable clinical research collaborations and trials.
Eventually we hope to provide opportunities for graduate students to join our teams working on projects related to perioperative cognitive dysfunction.
If you are interested in perioperative care or research, feel free to contact our department main office, or our Provincial Research Facilitator, Darcie Earle.
Peter Hedlin PhD, MD, FRCPCClinical Scientist
Assistant Professor
Dept. of Anesthesiology
University of Saskatchewan
Cardiac Anesthesia is a subspecialty of anesthesiology related to peri/intra and post-operative care of patients undergoing cardiothoracic surgeries. Cardiac Anesthesia poses significant clinical challenges given the invasive nature of surgery, patient population, and common physiologic instability.
Faculty: Ryan Pikaluk, Michele Clunie, Peter Hedlin, Eugene Choo
2. POCUS and Medical Education
Point of Care Ultrasound is the use of portable ultrasound as a diagnostic tool that leads to improved operational efficiency, expedited triage, shorted time to diagnosis, and improved patient outcomes.
Faculty: Michele Clunie, Lei Xia, Mateen Raazi, Paul Korchinski, Rob Perverseff, Eugene Choo, Henry Bi
3. Social/Gender Equity in Care
Equity of care is the absence of differences in care attributable to (perceived) differences among people groups defined by social, economic, cultural or geographic characteristics. Equity of care promotes equity in health outcomes.
We work closely with the Saskatchewan Center for Patient Oriented Research and our projects are enhanced by working with patients and patient families as our collaborators and Co-investigators.
Faculty: Michele Clunie, Mateen Raazi, Krissie Urmson
4. Quality Improvement
Quality Improvement research is an iterative process that collects and analyzes data on processes, interventions, and outcomes to promote ongoing evaluation and improvement in practice and performance.
Faculty: Malone Chaya, Lei Xia, Krissie Urmson, Peter Hedlin, Richard Schaan
5. Leadership and Health Care Systems
The study of Leadership in Health Care Systems ultimately aims to improve patient outcomes by improving the field of medicine and anesthesiology at a management and policy level. Research in this area generates data-driven observations, strategy development, and implementation frameworks for improving collaboration, processes, and outcomes at the level of the patient, clinician, individual, team and department level.
Faculty: Mateen Raazi, Lei Xia
6. Physician Wellness
Physician wellness or lack thereof, has an impact on the physician as well as on patient outcomes, and the health care system. Our research in this area explores consistent and novel stressors and challenges faced by physicians and residents, and works with physicians and residents to identify supports and solutions to avoiding burnout, anxiety and other mental and physical health concerns.
Faculty: Mateen Raazi, Joann Kawchuk, Anita Chakravarti, Richard Schann, Justina Koshinsky
7. Pediatrics
Pediatric anesthesiology is a subspecialty of Anesthesiology concerned with the care of children from newborn to adolescents, providing peri/intra and post-operative care to children, many who have complex medical problems affecting multiple organs and systems of the body.
Faculty: Jon Gamble, Krissie Urmson, Mateen Raazi
8. Critical Care
Critical care anesthesiologists work with patients in the intensive care unit, who have recently experienced surgery, trauma or severe infection, and require intravenous medication, monitoring heart activity, blood oxygen levels, blood pressure, respiratory and heart rate and modifying medication accordingly.
Faculty: Jon Gamble, Joann Kawchuk, Brian Brownbridge, Raj Brar
9. Peri-/Intra-operative Care
Peri(intra)operative care refers to the patient care provided surrounding a surgical event. Intraoperative care begins when the patient is transferred to the operating room and involves the administration of anesthesia to induces temporary unconsciousness, and/or eliminate (block) the pain sensation. Postoperative care comprises the time during which patients are still under anesthesia and admitted to the Post Anesthetic Care Unit (PACU) where they are monitored for vital stability and surgical complications.
Faculty: Malcom Lucy, Jon Gamble, Ryan Lett, Peter Hedlin, Brian Taylor
10. Regional Anesthesiology
Regional Anesthesiology is the administration of local anesthetic close to a nerve supplying and area of the body on which the surgery/procedure will occur. This includes epidural anesthesia for labor and delivery pain control.
Faculty: Churao Yang
Visit the Provincial Department of Anesthesiology Google Scholar page to find publications from our faculty and trainees.
Research resources for residents and faculty can be found on the Main Anesthesia Resident SharePoint site within the Resident Research folder
Note: The information on SharePoint is meant to be an internal resource for the deparment. It requires membership and a log in. If you need access, please contact Darcie Earle, Provincial Research Facilitator.
Dr. Jonathan Gamble
Executive Director Research
Dr. Peter Hedlin
Clinician Scientist
Dr. Jennifer O’Brien
Research Associate
Darcie Earle
Provincial Research Facilitator
Dr. Mary Ellen Walker
Statistician
Patient Information
Many of our patients have questions about our role as anesthesiologists as well as what types of anesthesia we can provide. Check out the links below to learn more:
Learn more about Cardiac Enhanced Recovery After Surgery (ERAS) for Patients: https://youtu.be/IdjebzaPbgo
Contact
Provincial Department of Anesthesiology
Royal University Hospital
G525-103 Hospital Drive
Saskatoon, SK
S7N 0W8
Phone: 306-655-1183
Fax: 306-655-1279
|
Manager, Administration & Finance
|
Brittany Minty Executive Assistant to Dr. Mateen Raazi, Provincial Head 306-655-1186 |
Teresa Krueger Scheduling Manager 306-655-1439 |
|
Clerical Assistant, Reception, and Clinical Support
|
|
|