Antibiotic management of prosthetic joint infections: review of current state and development of a clinical treatment pathway
Matthew Jarotski
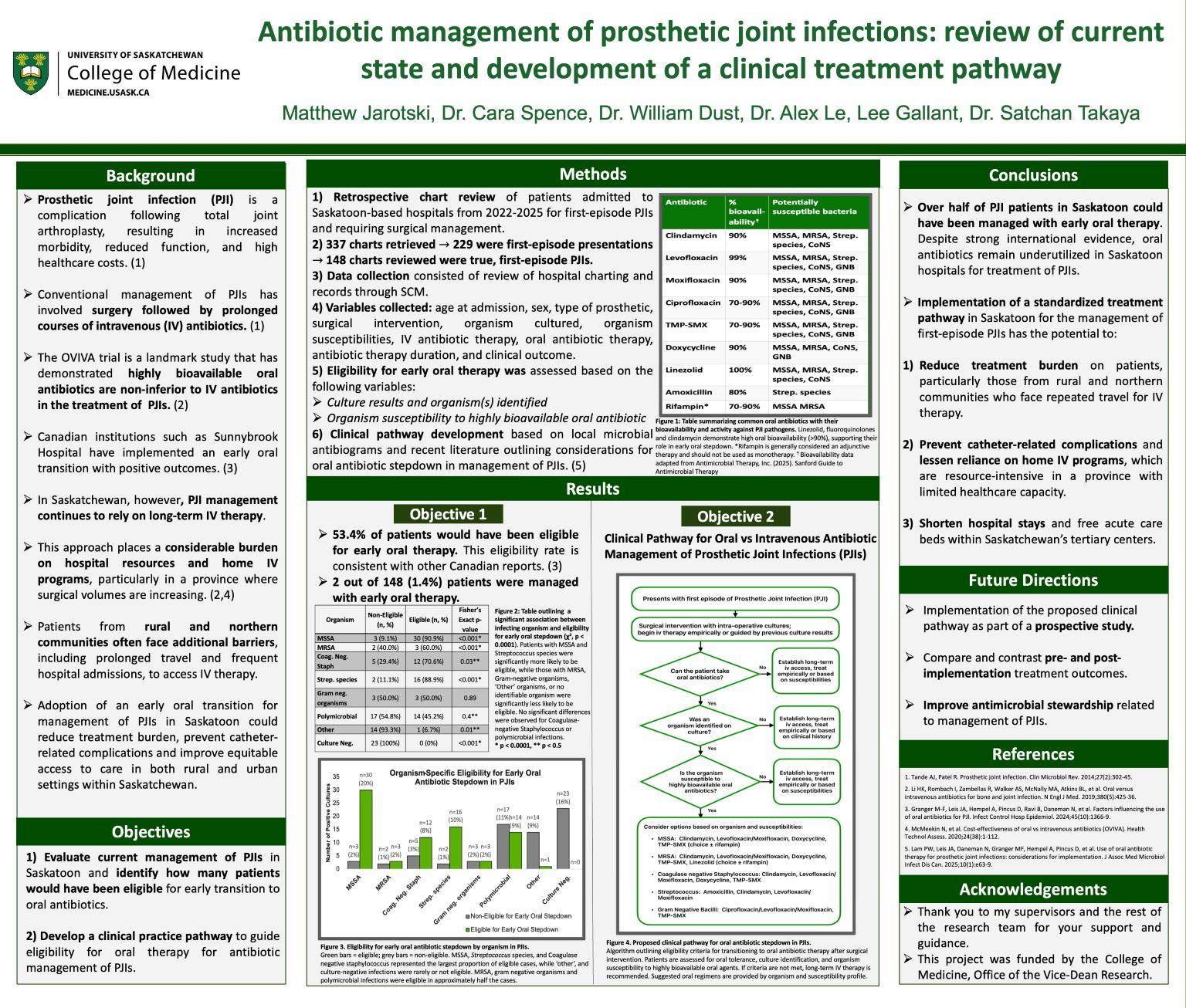
Prosthetic joint infection (PJI) is a serious complication of arthroplasty, traditionally managed
with prolonged intravenous (IV) antibiotic therapy (1,2). Recent evidence, including the OVIVA
trial, has shown that highly bioavailable oral antibiotics are non-inferior to IV therapy, while
reducing line-associated complications (3). The primary objective of this study was to evaluate
current management of PJIs in Saskatoon and to identify how many patients would have been
eligible for early transition to oral antibiotics. A retrospective review of patient charts with PJI
was conducted, of which 148 met eligibility criteria. Based on culture results and antibiotic
susceptibility, 79 patients (53.4%) were deemed appropriate candidates for an early oral step-down regimen. The secondary objective was to develop a clinical practice pathway to guide
eligibility for oral therapy. The pathway utilizes local microbial antibiograms, and emphasizes
surgical source control, organism susceptibility, and patient-specific considerations, aligning
with recent consensus statements supporting oral therapy in selected patients (4,5,6). The results
demonstrate that while over half of patients could be managed with early oral therapy, it remains
underutilized locally. Implementation of a standardized pathway may reduce treatment burden,
prevent catheter complications, reduce healthcare admission duration, and harmonize local
practice with current international evidence for antibiotic management of PJIs (3,7,8,9).
