HIV Post Exposure Prophylaxis (PEP) Prescribing in Saskatoon Emergency Departments: Pre and Post CME Intervention
Jasmin Ogren
Introduction: Saskatchewan has the highest incidence of HIV in Canada, driven by inequities that disproportionately affect Indigenous peoples and those in rural and northern communities. HIV post-exposure prophylaxis (PEP) prevents HIV and must be initiated within 72 hours of exposure. Emergency departments (EDs) are often the first point of care following sexual assault or needlestick injury. As coverage for PEP required approval by an ID specialist or Designated ARV Prescriber, CME was developed to onboard ED prescribers.
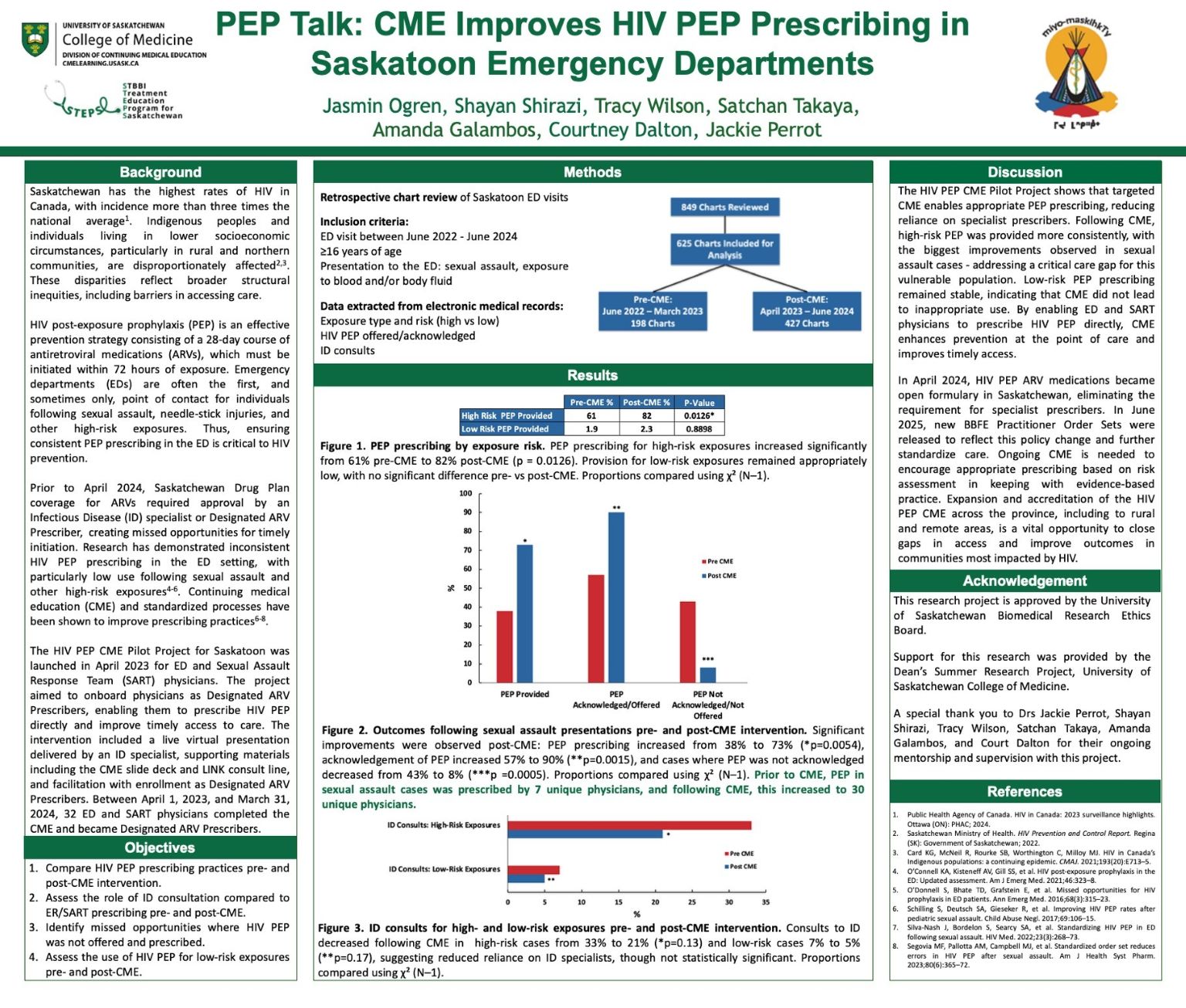
Methods: A retrospective pre-post chart review evaluated the impact of a CME intervention for ED and Sexual Assault Response Team physicians on PEP prescribing in Saskatoon EDs. 625 charts met inclusion criteria: patients ≥16 years presenting after sexual assault or blood/body fluid exposure.
Results: PEP prescribing for high-risk exposures increased from 61% pre-CME to 82% post-CME (p = 0.0126). In sexual assault cases, PEP prescribing increased from 38% to 73% (p=0.0054), acknowledgement of PEP increased 57% to 90% (p=0.0015), and cases not acknowledged decreased from 43% to 8% (p =0.0005).
Conclusion: Targeted CME enables appropriate PEP prescribing, reducing reliance on specialist prescribers. High-risk prescribing improved significantly, particularly following sexual assault. CME strengthens HIV prevention at the point of care and improves access.
