Survival Impact of Coexisting Diabetes in Pancreatic Cancer: A Saskatchewan Population Based Cohort Study
Omer Munir
Background: Diabetes mellitus (DM) is both a risk factor for and a potential consequence of pancreatic ductal adenocarcinoma (PDAC). Its prognostic role remains uncertain. This study examined the impact of DM on outcomes in a population-based cohort.
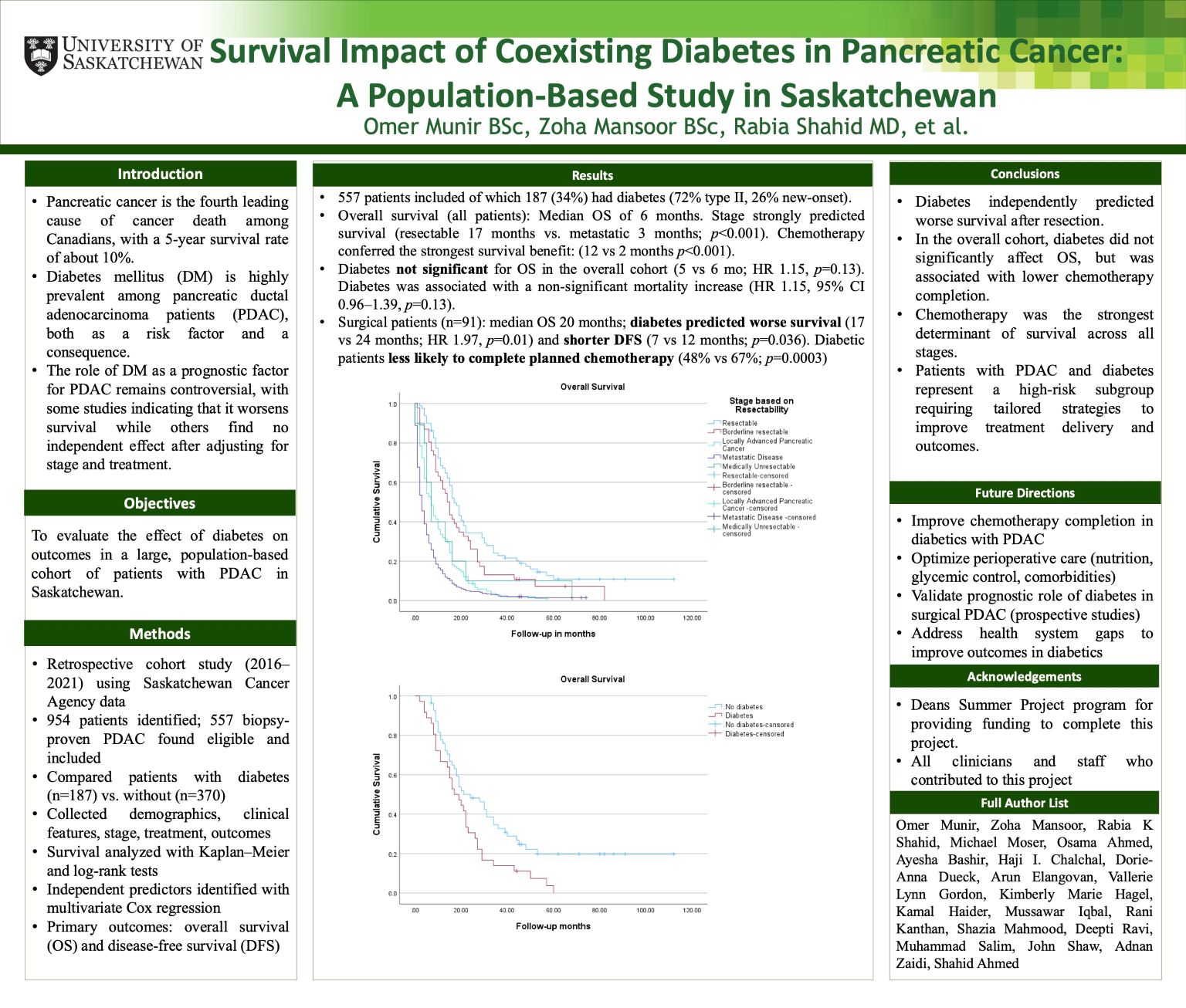
Methods: We performed a retrospective cohort study of biopsy-proven PDAC diagnosed in Saskatchewan (2016–2021). Kaplan–Meier estimates were compared with log-rank testing, and Cox regression identified predictors of overall survival (OS) and disease-free survival (DFS).
Results: Among 954 identified patients, 557 were eligible; 187 (34%) had DM. Diabetic patients were older, had more comorbidities, and longer symptom duration. Surgery was performed in 91 patients, including 36 with DM. In this subgroup, DM predicted inferior DFS (7 vs. 12 months, p=0.036) and OS (17 vs. 24 months, p=0.01), with multivariate analysis confirming DM as an independent risk factor (HR 1.97, 95% CI 1.17–3.32). Chemotherapy significantly improved DFS (13 vs. 4 months) and OS (24 vs. 9 months), but completion rates were lower among diabetics (48% vs. 67%, p=0.0003). In the full cohort, chemotherapy remained the strongest determinant of survival (median OS 12 vs. 2 months).
Conclusions: Diabetes predicted worse survival after resection and reduced treatment completion. Chemotherapy conferred the greatest survival benefit, underscoring the need for tailored strategies in diabetic PDAC patients.
