Learning Clinical Reasoning and Evidence-Based Medicine in USask Undergraduate Medical Education: Are We Meeting Our Goals?
Johann Morhart
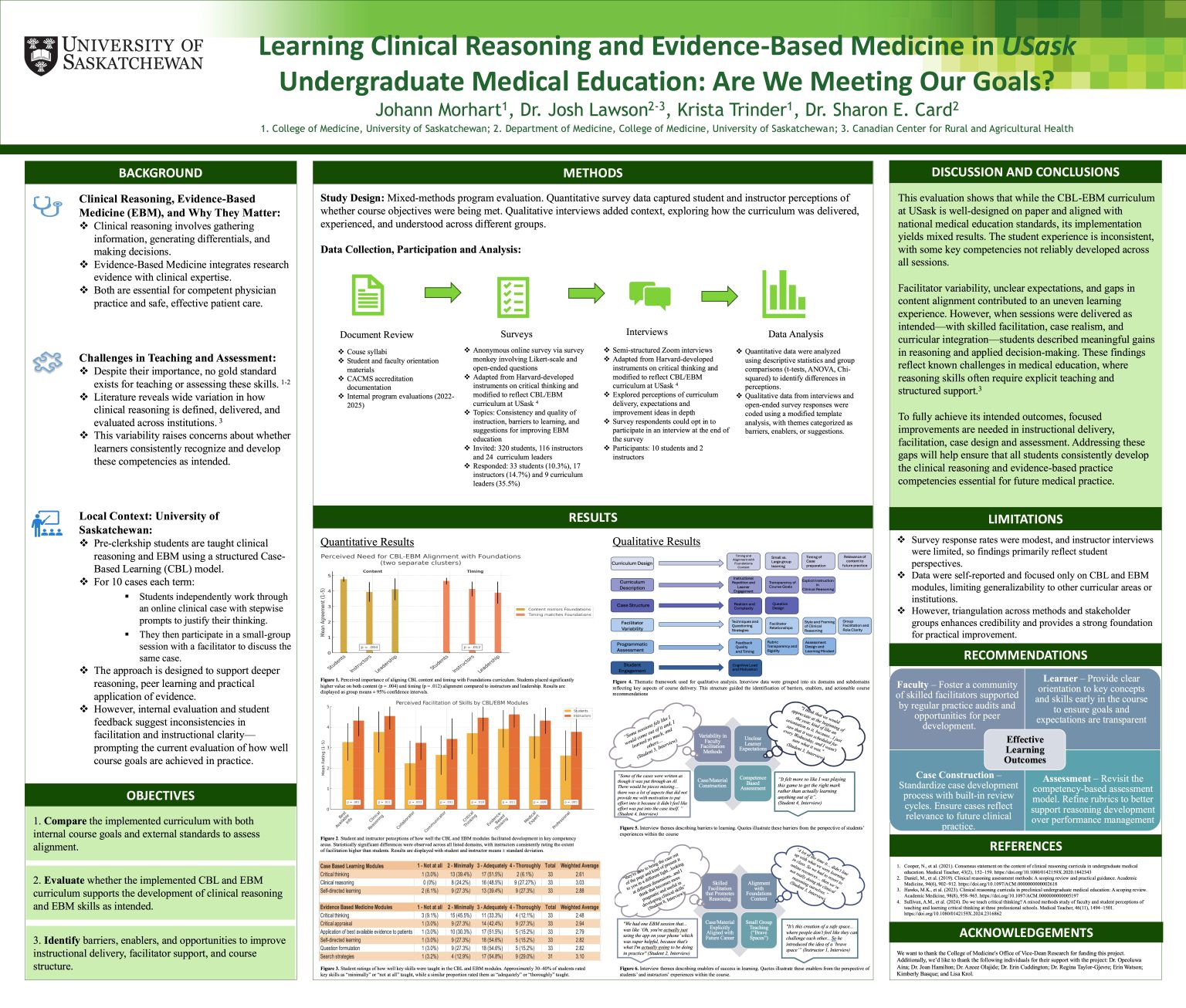
Background: Clinical reasoning and evidence-based medicine (EBM) are essential competencies in medical education, taught at USask through pre-clerkship Case-Based Learning (CBL) and EBM modules. Internal feedback raised concerns about inconsistent delivery and instructional alignment.
Methods: We conducted a mixed-methods program evaluation. Surveys were distributed to pre-clerkship students, small-group facilitators, and curriculum leaders to assess whether teaching aligned with intended learning outcomes. Semi-structured interviews with students and instructors explored how sessions were delivered and experienced.
Results: Surveys revealed perception gaps between students and faculty. Instructors rated the teaching of key skills significantly higher than students did, while students placed greater value on alignment between cases and other course content. Qualitative interviews identified key barriers: inconsistent facilitation, unclear expectations, poorly timed or unrealistic cases, and grading structures that discouraged exploration and reasoning development. Conversely, sessions with engaged facilitators, well-aligned cases, and supportive environments were seen as highly effective.
Conclusions: Although the CBL-EBM curriculum aligns with national educational standards, its implementation is inconsistent. Variability in facilitation, case design, and assessment limits students’ ability to reliably develop clinical reasoning and EBM skills. Targeted improvements such as faculty development, clearer orientation, standardized case design, and revised assessment are recommended to better support intended learning outcomes.
