Physician Perspectives of Opioid Agonist Therapy Prescribing and Suboxone Macrodosing in the Emergency Department: A mixed methods study
Mirza (Sarim) Asim
Background: Emergency-department initiation of buprenorphine/naloxone (bup/nal) reduces opioid-related harm, yet uptake of bup/nal prescribing and use of a newly developed macrodosing practitioner pre-order set (PPO) remain uncertain.
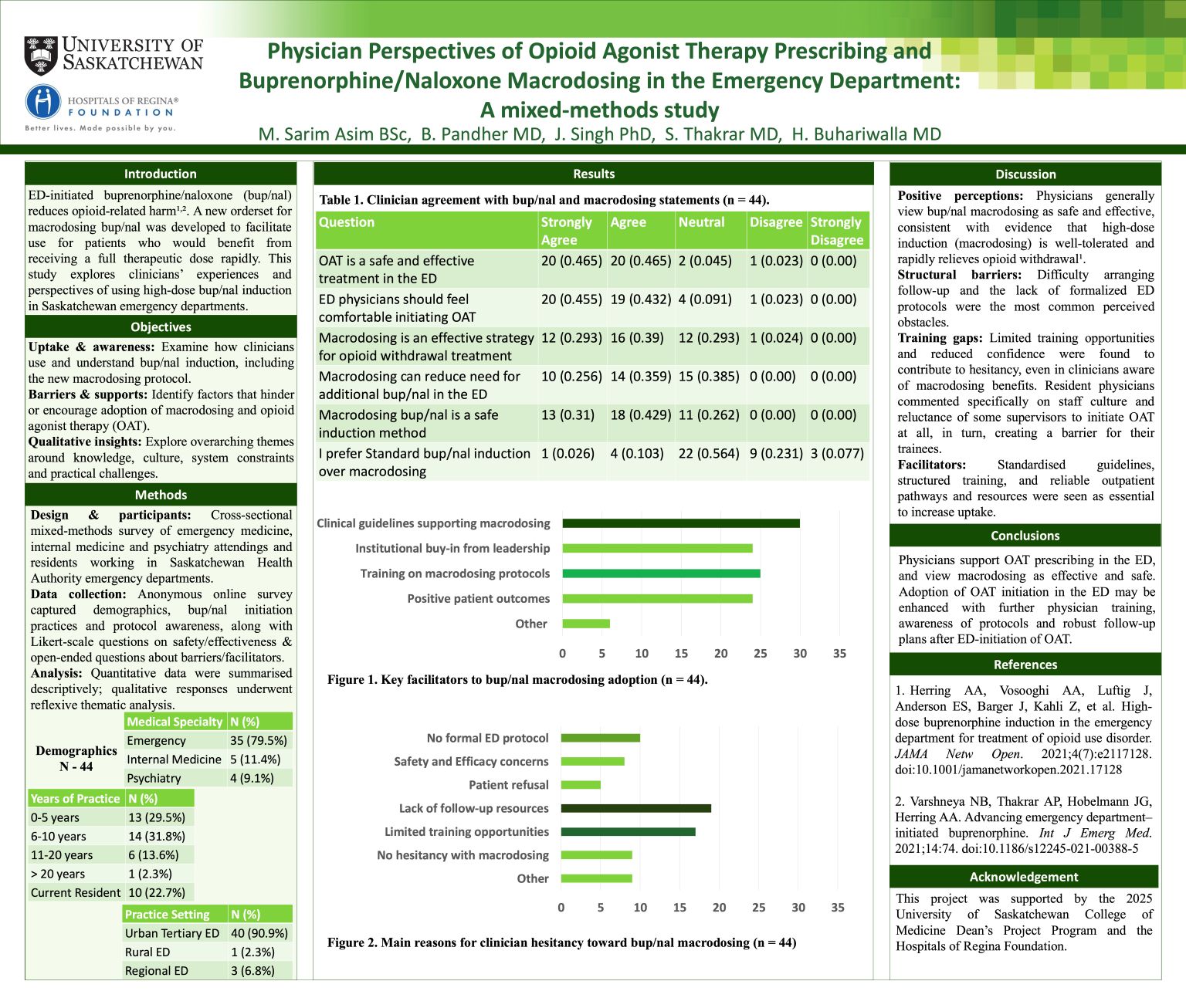
Methods: A cross-sectional, mixed-methods survey was administered to physicians and residents from emergency medicine, internal medicine, and psychiatry across Saskatchewan Health Authority emergency departments. The questionnaire collected demographics, knowledge and attitudes toward opioid agonist therapy (OAT) and induction strategies (standard, micro- and macrodosing), as well as open-ended responses on barriers and facilitators. Quantitative data were analyzed descriptively, and qualitative responses underwent reflexive thematic analysis using Braun and Clarke’s six-step approach.
Results: Forty-four physicians responded; 35/44 (79.5%) were emergency physicians at urban tertiary care settings. Of the 33 who had initiated bup/nal: 15 used macrodosing, 13 standard induction, and 5 micro-dosing. Barriers to initiating OAT were inability to arrange follow-up and lack of comfort. Hesitancy toward macrodosing stemmed from limited follow-up resources, training opportunities, and lack of formal ED protocols. Qualitative themes reflected knowledge gaps, systemic barriers, and concerns about precipitated withdrawal and monitoring in crowded emergency departments.
Conclusions: Physicians generally support bup/nal initiation and acknowledged macrodosing as a safe and effective approach, yet uptake remains constrained by training deficits, absent protocols, and inadequate follow-up infrastructure.
