Polypharmacy and 1-year prognosis in persons referred to a rural and remote memory clinic
Elliot Grande-Sherbert
Background: Polypharmacy, the use of ≥5 regular medications, is common in rural older adults and those with dementia.
Objective: To evaluate the relationship between number of medications and one-year change in cognition, function, and behaviour among rural-dwelling older adults referred to a memory clinic.
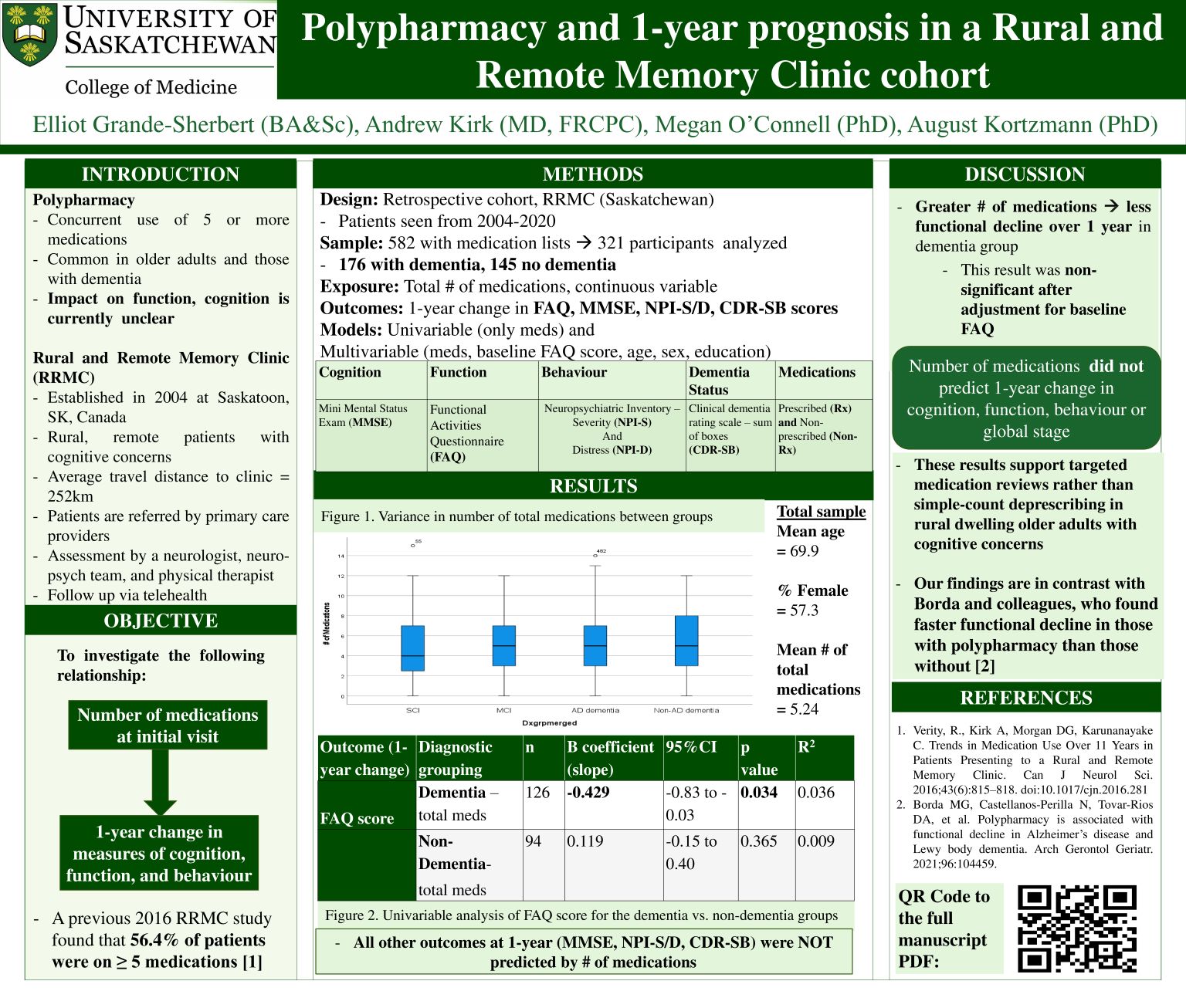
Methods: We conducted a retrospective cohort study of patients assessed at the Rural and Remote Memory Clinic (RRMC) in Saskatoon, Saskatchewan, Canada from 2004-2020. Baseline medication burden was examined as a predictor for 1-year change in the Mini-Mental State Exam (MMSE), Functional Activities Questionnaire (FAQ), Neuropsychiatric Inventories (NPI-S, NPI-D), and Clinical Dementia Rating Scale, Sum of Boxes (CDR-SB).
Results: A total of 321 patients were included (mean medication count 5.2). In those with dementia, higher prescription count was associated with a 0.43 smaller rise in FAQ score (B = -0.43, 95% CI: -0.83 to -0.03, p=0.034). After adjusting for baseline FAQ, this association was attenuated and no longer significant (B =-0.36, 95%CI: -0.73 to 0.01, p=0.055, R2=0.168, n=125). No other significant associations were observed.
Conclusion: Number of medications did not predict cognitive, behavioural, or functional outcomes. Findings support routine medication reviews and rational deprescribing in rural older adults.
