Stroke is a major killer and number one cause of long-term disability facing Canadians today. Research focused on individuals with stroke and other cerebrovascular diseases must translate into meaningful improvements in prevention, diagnosis, treatment and rehabilitation. The result being a reduction of the devastating effects associated with these conditions.
The Saskatchewan Cerebrovascular Center began in 2008. Under the University of Saskatchewan, endovascular neurosurgical services and associated clinical research trials became a reality in this province. Prior to the centers inception, patients had to be treated, often on an urgent basis, at already established cerebrovascular centers across Canada.
Medical professionals have long agreed that cerebrovascular diseases and disorders including acute stroke, aneurysms and arteriovenous malformations are amongst the most challenging conditions to treat. Novel and state of the art therapies expertly delivered at the Saskatchewan Cerebrovascular Center focus on providing superior treatment and care to this patient group.
To stay current in the treatment of stroke and cerebrovascular disorders, the Centre has become involved in 15 multicentre clinical trials. It is imperative that patients receive proven up to date treatments. The program extensively utilizes the services of the Saskatoon Centre for Patient Oriented Research to ensure this is a reality.
Basic science stroke research is performed using a collaborative approach. Director Dr. Michael Kelly is a member of the CIHR/HSFC Team in synchrotron medical imaging. The goal of his research program is to perform bench to bedside testing of medical devices and other therapies such as stem cell treatment for stroke.
The Saskatchewan Cerebrovascular Centre continues to grow, attracting many high quality personnel to the University of Saskatchewan including a second endovascular/cerebrovascular neurosurgeon, multiple research nurses, post-doctoral fellows and administration officials. The Centre is succeeding to fulfill its mandate by providing leading treatments and being a key player in the field of stroke and cerebrovascular research.
What is Stroke?
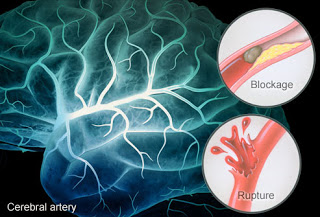
A stroke is a sudden loss of brain function. It is caused by the interruption of flow of blood to the brain (ischemic stroke) or the rupture of blood vessels in the brain (hemorrhagic stroke). The interruption of blood flow or the rupture of blood vessels causes brain cells (neurons) in the affected area to die. The effects of a stroke depend on where the brain was injured, as well as how much damage occurred. A stroke can impact any number of areas including your ability to move, see, remember, speak, reason and read and write.
What are the stroke warning signs?
Stroke can be treated and it is important to recognize the warning signs, even if temporary:
- Sudden weakness, loss of strenght or numbness in the face, arm or leg
- Sudden difficulty speaking
- Sudden vision problems
- Sudden severe, unusual headache
- Sudden dizziness/loss of balance, especially if combined with any of the above symptoms.
What are the types of stroke?
- Ischemic stroke is caused by the interruption of blood flow to the brain due to a blood clot.
- Hemorrhagic stroke is caused by uncontrolled bleeding in the brain.
- Transient ischemic attack (TIA) or mini-stroke preceds a major stroke. Many people experience fleeting stroke symptoms, called transient ischemic attack, or a TIA. A person who has had one or more TIAs is almost 10 times more likely to have a stroke than someone of the same age and sex who has not. Unfortunately, TIAs are often undiagnosed and unreported. Studies in Canada have shown that rapid assessment and follow-up of an individual experiencing a TIA can prevent a major stroke.
Understanding the brain and the effects of stroke
Your brain is the most complex organ in your body. It consists of more than 100 billion specialized nerve cells called neurons and it acts as a command centre for everything you do, think, sense and say. These neurons depend on the blood vessels in your brain for oxygen and nutrients. Neurons cannot duplicate or repair themselves.
Different parts of the brain control different functions. When someone has a stroke, the functions that are affected depend upon which area of the brain was damaged and how much damage occurred. Learning what the different parts of the brain do can help you understand why the effects of stroke can be so different among different people.
What is Brain Aneurysm?
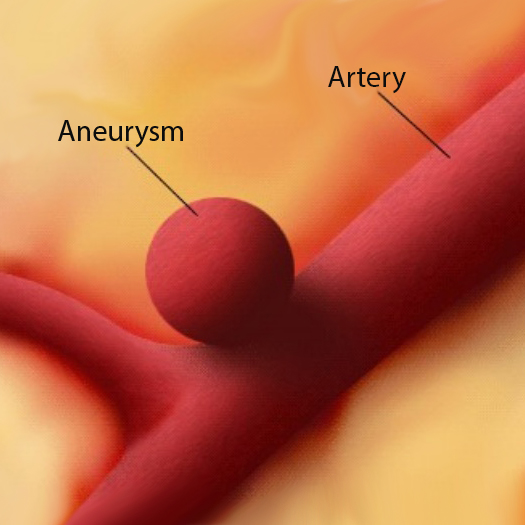
An aneurysm is an abnormal, weak spot on a blood vessel that causes an outward bulging or ballooning of the arterial wall. These weak spots can involve all walls of the blood vessel (fusiform aneurysm), form a sac from one wall (saccular) or separate the vessel walls (dissecting). An aneurysm can affect any vessel in the body but only those in the head can cause a serious medical condition, a hemorrhagic stroke when they rupture, which can lead to brain damage and death.
Brain aneurysms are often discovered when they rupture, causing bleeding into the brain or the space closely surrounding the brain called the subarachnoid space, causing a subarachnoid hemorrhage. Subarachnoid hemorrhage from a ruptured brain aneurysm can lead to a hemorrhagic stroke, brain damage and death.
The main goals of treatment once an aneurysm has ruptured are to stop the bleeding and potential permanent damage to the brain and to reduce the risk of recurrence. Unruptured brain aneurysms are sometimes treated to prevent rupture.
Incidence Rates of Brain Aneurysms
- Brain aneurysms are an uncommon disorder of the blood vessels that are usually acquired with age and affect approximately 5% of Canadian population.
- The annual incidence of aneurysmal subarachnoid hemorrhage in Saskatchewan exceeds 100 people. Ten to 15 percent of these patients will die before reaching the hospital and over 50 percent will die within the first thirty days after rupture. Of those who survive, about half suffer some permanent neurological deficit
- The most significant risk factors are cigarette smoking and having a close relative who had an aneurysm.
- The average age at presentation is usually 50 to 60 years old.
- Aneurysms are found more commonly in females than in males (3:2), and 20% of patients have multiple (two or more) aneurysms.
Diagnostics and Treatment
If you have symptoms that could be stroke-related, or have risk factors for stroke, your doctor may conduct a number of tests to help with your diagnosis and treatment. Your doctor will first determine if you have had a stroke, and if so, what type of stroke you experienced. Your doctor will also determine what parts of your brain have been affected. Here are some of the diagnostic tests that will be conducted if you have symptoms of a stroke:
- Angiography or arteriography
- Blood test and urine test
- Carotid ultrasound (Doppler)
- CT or CAT scan
- Echocardiogram
- Electrocardiogram
- Electroencephalogram (EEG)
- Holter or event monitoring
- Magnetic Resonance Imaging (MRI)/Magnetic Resonance Angiography (MRA)
- Neurological exam
- Physical exam
- Transesophageal echocardiogram (TEE)
Treatment
There are three main emergency treatments for stroke: tPA, surgery and non-surgical procedures. The treatment you receive will depend on the type of stroke, how serious the stroke was, the age and general health, and how soon the patient arrives at the hospital. About 80 percent of stroke patients have blocked arteries in the brain that starve part of the brain of its blood supply. In the other 20 percent of stroke patients, blood vessels burst as the result of an abnormal outpouching of an artery, an aneurysm, or a ruptured small artery.
Saskatchewan Cerebrovascular Centre specialists assess patients rapidly to determine the cause of the stroke. If an artery is blocked, several treatment options are available, but speed is essential because the brain rapidly dies when deprived of blood. tPA (tissue plasminogen activator) is a drug that can stop a stroke caused by a blood clot by breaking up the clot. tPA is short for tissue plasminogen activator and can only be given to patients who are having a stroke caused by a blood clot (ischemic stroke). It must be given within 4½ hours of the onset of symptoms.
In some cases, surgery may be required to repair damage after a stroke or to prevent a stroke from occurring. Surgery may be performed to remove blood that has pooled in the brain after a hemorrhagic stroke, to repair broken blood vessels, or to remove plaque from inside the carotid artery.
For patients with bleeding from an aneurysm, new endovascular procedures, which work inside the blood vessels, enable surgeons to operate on the brain without opening the skull (craniotomy). In some patients bleeding arises from an abnormal tangle of arteries and veins, called an arteriovenous malformation. This condition can also be treated with an endovascular approach, sparing patients the risk, discomfort and longer hospitalization of a craniotomy.
EndovascularTreatment of Stoke: In addition to tPA
Patient Education
Stroke occurs when the blood supply to part of the brain is cut off. Without oxygen-rich blood, brain cells begin to die. If the blood supply is not restored, the affected part of the brain dies, causing disability or death. You can't control your family history, age, gender or ethnicity but you can do something about other factors that could increase your risk of having a stroke:
- Check your blood pressure (hypertension): High blood pressure is a major stroke risk factor if left untreated. Have blood pressure checked yearly by a doctor or at health fairs, a local pharmacy or supermarket or with an automatic blood pressure machine.
- Identify atrial fibrillation (Afib): Afib is an abnormal heartbeat that can increase stroke risk by 500%. Afib can cause blood to pool in the heart and may form a clot and cause a stroke. A doctor must diagnose and treat Afib.
- Stop smoking: Smoking doubles the risk of stroke. It damages blood vessel walls, speeds up artery clogging, raises blood pressure and makes the heart work harder.
- Control alcohol use: Alcohol use has been linked to stroke in many studies. Most doctors recommend not drinking or drinking only in moderation - no more than two drinks each day.
- Know cholesterol levels: Cholesterol is a fatty substance in blood that is made by the body. It also comes in food. High cholesterol levels can clog arteries and cause a stroke. See a doctor if your total cholesterol level is more than 200.
- Control diabetes: Many people with diabetes have health problems that are also stroke risk factors. A doctor and dietician can help manage diabetes.
- Manage diet/exercise: Excess weight strains the circulatory system. Exercise five times a week. Maintain a diet low in calories, salt, saturated and trans fats and cholesterol. Eat five servings of fruits and vegetables daily.
- Treat circulation problems: Fatty deposits can block arteries carrying blood to the brain and lead to a stroke. Other problems such as sickle cell disease or severe anemia should be treated.
- Transient Ischemic Attack: A TIA is a temporary episode of stroke-like symptoms that can last a few minutes to 24 hours but usually causes no permanent damage or disability. TIA and stroke symptoms are the same. Recognizing and treating a TIA can reduce stroke risk. Up to 40 percent of people who experience a TIA may have a stroke.
Research Group
Learn more about the Saskatchewan Cerebrovascular Centre research group members, ongoing studies and more by visiting the SCVC website.
Our Team
Neurosurgery
Michael Kelly, MD, PhD, FRCSC, FACS, FAANS - Professor, Head of Neurosurgery
Lissa Peeling, BSc, MD, FRCSC - Associate Professor, Neurosurgery
Stroke Neurology / Neurocritical Care
Gary Hunter, MD, FRCP(C), CSCN(EEG) - Assistant Professor, Neurology
Brett Graham, MD, FRCP(C) - Assistant Professor, Neurology
Sanchea Wasyliw, MD, FRCP - Assistant Profesor, Neurology
Regan Cooley, MD, FRCP(C) - Assistant Profesor, Neurology
Neuroradiology
Peter Szkup, MD, FRCP(C)
Rob Otani, MD, FRCP(C)
Kyle Molton, MD, FRCP(C)
Johnathan Grynspan, MD, FRCP(C)
Nursing
Aaron Gardner, RN, BSN, CNN(c)
Ruth Whelan, RN, BSN, MN, CNN(c)
Jodi Copeland, RN, BSN, CNN(c)
Basic Science Research
Jake Pushie, PhD
Nicole Sylvain, MSc
Huishu Hou, MSc
Saskatchewan Health Authority Administration
Lisa Korec, RN, BN, CON(C) - Provincial Director of Neurosciences
Andrea Kleiter, RD - Manager of Outpatient Neurosciences
Contacts
Dr. Michael Kelly
(306) 655-2354
Saskatoon SK S7N 0W8
Dr. Lissa Peeling
(306) 655-1333Saskatoon SK S7N 0W8
Aaron Gardner, RN
(306) 655-2354
Saskatoon SK S7N 0W8
