Improving Pain Recognition in Saskatchewan ICUs
Memoon Qureshi
Pain is one of the most common and distressing symptoms in the ICU, with up to 79% of patients reporting moderate to severe pain. Sedated or non-communicative patients also experience pain, and untreated pain has been linked to higher mortality among other consequences. The PADIS guidelines recommend structured and multimodal strategies for pain assessment, with validated behavioral tools such as the Critical-Care Pain Observation Tool (CPOT) for patients unable to self-report.
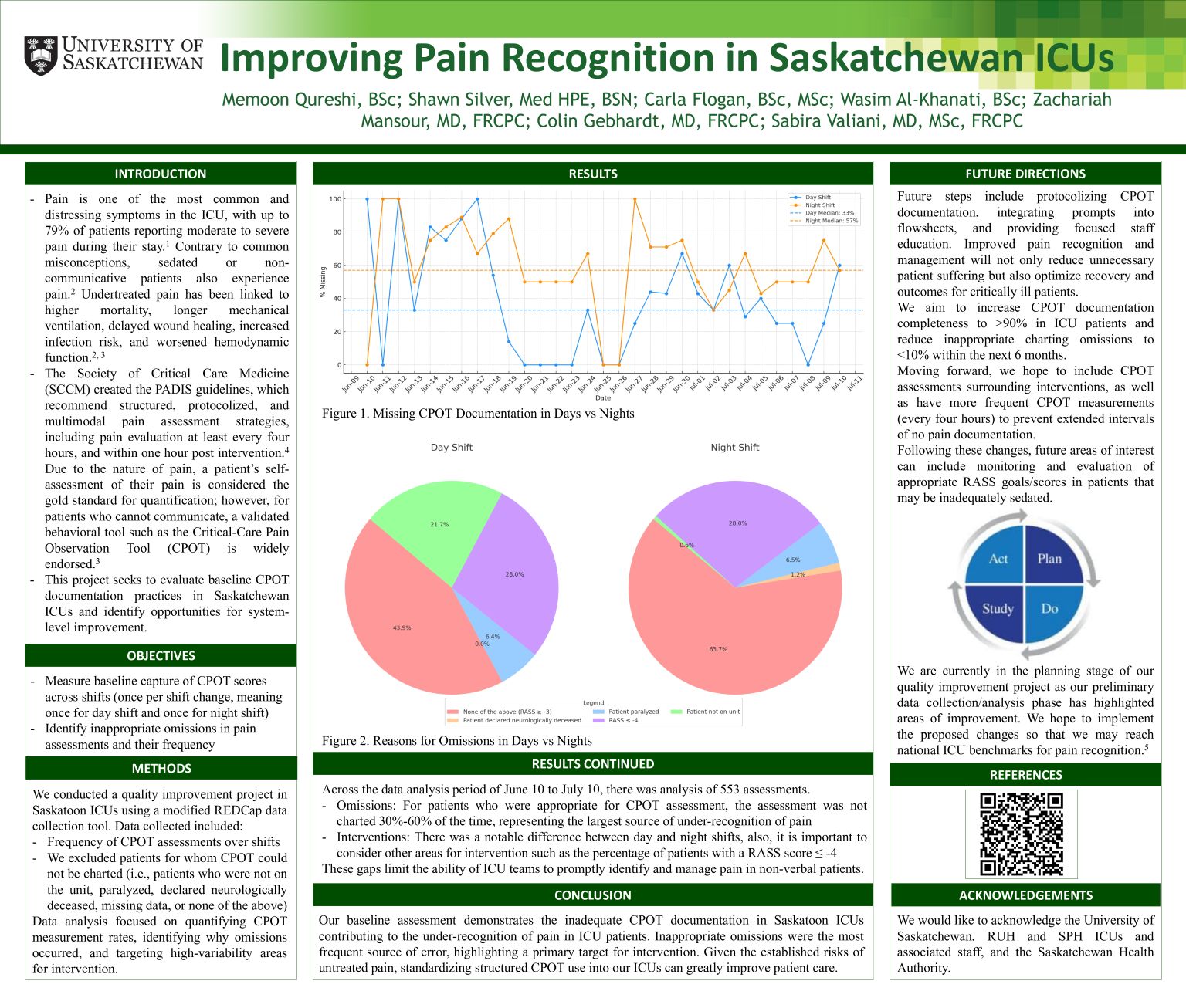
This quality improvement project evaluated baseline CPOT documentation practices in Saskatoon ICUs to identify opportunities for improvement. Using a modified REDCap tool, we collected data on the frequency of CPOT assessments, appropriateness of omissions, and variability across day and night shifts.
Across 553 assessment opportunities, between 30%-60% were omitted without valid justification. These errors were vastly different between day and night shifts and constituted the primary barrier to reliable pain recognition.
This baseline assessment highlights inadequate CPOT documentation, leading to under-recognition of pain in critically ill patients. Quality improvement efforts will focus on standardizing CPOT use, integrating prompts into workflows, and providing targeted staff education, with the aim of increasing documentation completeness and reducing inappropriate omissions.
