Working to understand harm reduction in Saskatoon
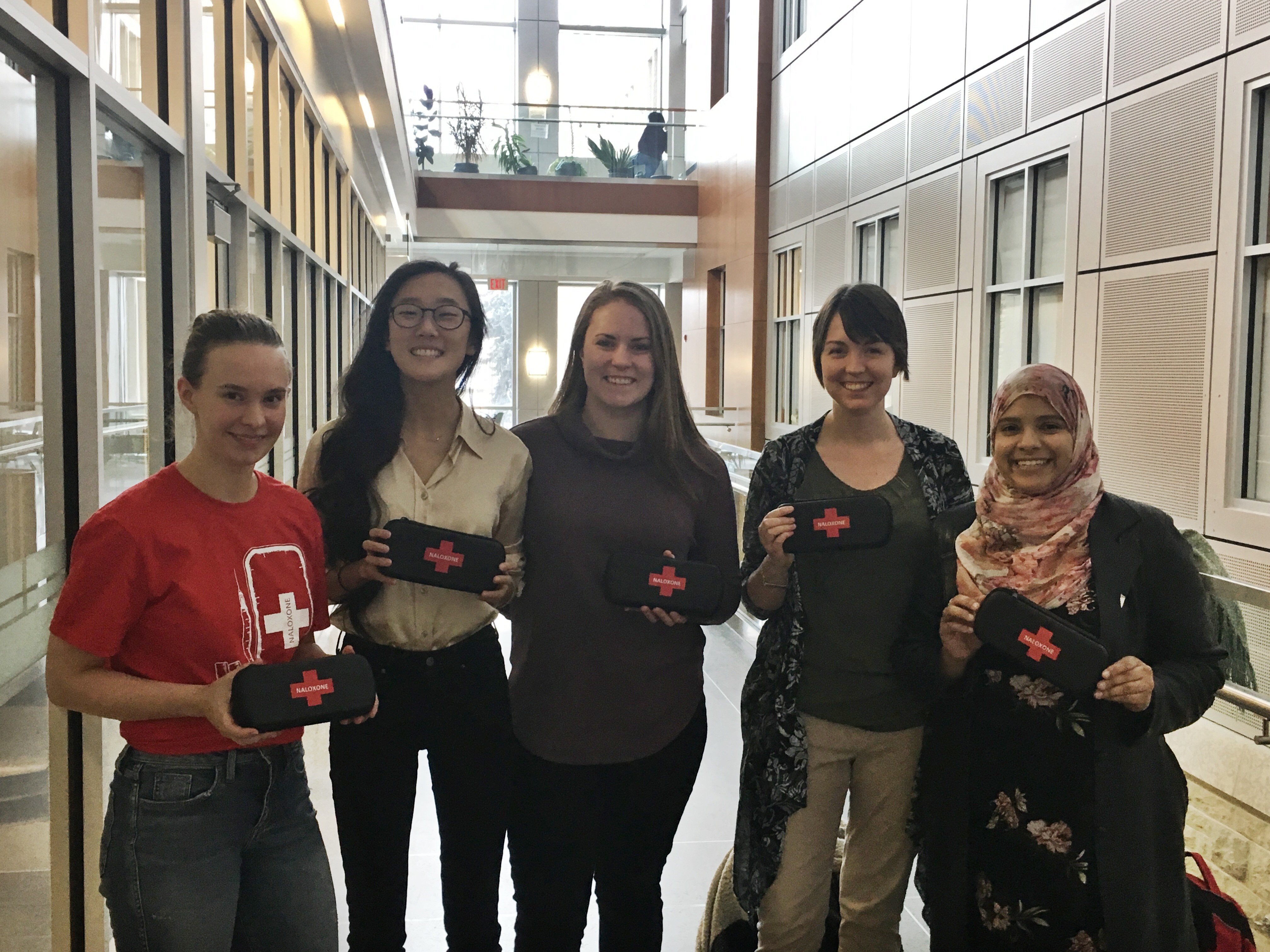
In the hustle and bustle before a long stretch of back-to-back finals, myself and fellow U of S students took a step back from our studying to be trained in recognizing and responding to an opioid overdose, including education on naloxone administration.
By Jessica FroehlichAIDS Saskatoon has worked tirelessly to advocate for the deregulation of naloxone, so that more people can have access to the kits and the training that reduces stigma and saves lives. Previously, the kits were only available through the Saskatchewan Health Authority and certain pharmacies, and training was offered at specific times.
I am extremely grateful to USSU Help Center Coordinator, Elizabeth Plishka, for organizing the opportunity and promoting the importance of this training to students and faculty on campus. Preventative measures and education such as this are needed to prepare Saskatchewan for the opioid crises seen across B.C, Alberta, and Ottawa.
The naloxone kits are not a replacement for substance use treatment, but they do save lives by allowing people who have overdosed enough time to be transported to a hospital. There’s a quote I like that states, “The only thing naloxone enables is breathing.”
So, what exactly is naloxone? It is an opioid antagonist, which means that it blocks the actions of opioid drugs by competing for the receptors they bind to in the brain. If a person has overdosed on an opioid drug such as heroin, morphine or opium – and is not breathing –administering naloxone can reverse those effects. Additionally, some opioid and non-opioid drugs are laced with fentanyl, unbeknown to the person taking them. Fentanyl is an extremely strong opioid and a tiny grain can be fatal.
The naloxone training occurred during Canada’s HIV/AIDs Awareness Week, where many physicians and community leaders gave talks on the matter. The SMSS Global Health Committee hosted a lunchtime talk with Jason Mercredi, executive director of AIDs Saskatoon. After his discussion, I have been reflecting more on the philosophy of harm reduction and what it encompasses holistically.
We all practice harm reduction every day. As a young dancer, I learned how to warm up properly and land my jumps in a deep plié to prevent injuries. As a lifeguard, I enforced the ‘no running’ rule to prevent falls and I taught swimming lessons to prevent drowning. But when we think of harm reduction, we only think of clean needle exchanges and wearing bike helmets or seat belts – we think of the physical.
Mercredi discussed broadening our views of harm reduction so that they are more comprehensive than a health and public safety philosophy. We must not only do our part to help reduce the harms of drug use but help to reduce the harms of the traumas that so often lead to substance misuse.
Plenty of research shows that the social determinants of health have lifelong effects on people’s brain development and ability to cope with adverse events. Often, mental illness and substance use are consequences of early childhood traumas. They are coping mechanisms that offer a person a sense of control and relief from their pain. We must take a look at where people’s suffering is stemming from.
Harm reduction includes investing in the social determinants as a community and fostering conditions to promote healing. This includes taking on poverty, racism, and colonialism. In Saskatchewan, it could mean improving working conditions or reducing the number of children in care.
With my medical student cap on, I could tell you all about how harm reduction in the form of clean needles and education can prevent abscesses, osteomyelitis, endocarditis, Hepatitis C, and HIV. But it can also reduce stigma, it can help people heal on their own terms, and it can promote self-love.
