Welcome
The Division of Neurosurgery is at the forefront of innovative basic science and clinical-translational research. To foster innovative solutions for world-class neurosurgical patient care, we have developed highly successful research programs across the spectrum of our mandate, including stroke, spine, pediatrics, oncology and functional neurosurgery. By harnessing the latest advances in the lab, we have been able to offer some of the latest clinical treatments for Saskatchewan patients.

Saskatchewan Cerebrovascular Centre
Primary Investigators
Michael Kelly, MD, PhD, FRCSC, FACS, FAANS
Lissa Peeling, BSc, MD, FRCSC
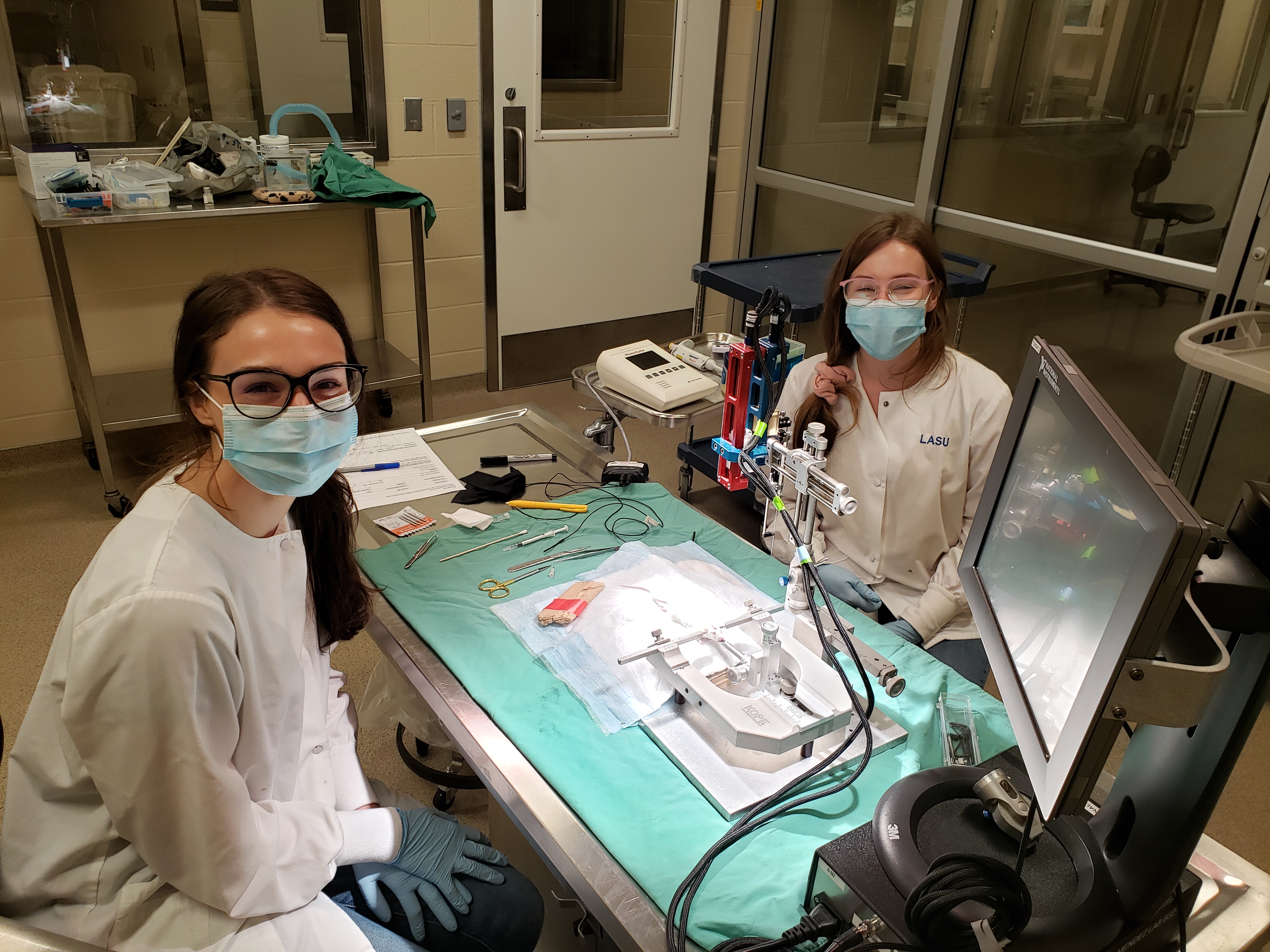
Our research program focuses on metabolic changes in the brain following disease or injury. We employ a combination of traditional biological laboratory techniques, including histology and immunohistochemistry, with advanced synchrotron-based imaging techniques. These methods allow our team to visualize subtle changes in the metabolic state of tissues and characterize changes that occur anywhere from the atomic to the anatomic level. Our advanced imaging methods include Fourier transfer infrared (FTIR) spectroscopic imaging, a method that allows us to visualize changes at the molecular level, and X-ray fluorescence imaging (XFI), which allows us to map a wide range of elements at their naturally occurring levels.
The team has surgical expertise in rodent stroke models, including hypoxic ischemia (HI), the photothrombotic (PT) model, and the middle cerebral artery occlusion (MCAO) model, as well as a collagenase mouse model of intracerebral hemorrhage (ICH).
Recent areas of investigation have included:
• Characterizing the changes in metabolic markers over time following onset of ischemic stroke
• Effects of the drug trifluoperazine on stroke lesion size and post-stroke edema
• New methods for data reduction, statistical analysis and clustering for imaging data
• Differences in size and brain metabolic response to ischemic stroke in male and female subjects
• Identifying new markers to characterize and track hemorrhagic transformation of ischemic stroke
• The effects of elevated iron status on stroke severity and post-stroke oxidative damage in the brain
Learn more by visiting the Saskatchewan Cerebrovascular Center Website.
Applied Neurosurgery Research Laboratory

Primary Investigator
Jonathan Norton, PhD, BSc(HONS), MRes, FACNS
The Applied Neurophysiology Research Laboratory, under PI Dr Jonathan Norton, investigates methods to make surgery safer and understand neurophysiological signals recorded during surgery and other acute procedures. This includes understanding the physiological basis of routine tests such as pedicle screw testing, (Norton et al 2021) and novel analysis of signals recorded during surgery (Norton et al 2018, Kelly et al 2021).
The lab also is involved in the development of neuromodulation/neuroprostheses, including understanding the mechanisms of action of spinal cord stimulation and the development of novel stimulation paradigms. We also work to understand the interactions between electrical stimulation and the nervous system (Norton 2021) as well as neurophysiological markers of pathology.
Presurgical Neuroimaging Program
Primary Investigator
Layla Gould, PhD
The Presurgical Neuroimaging Program at RUH is led by Dr. Layla Gould and the primary team members include Dr. Ron Borowsky (Professor, Dept. Psychology), Dr. Marla Mickleborough (Assistant Professor, Dept. Psychology), Josh Neudorf (PhD student, Dept. Psychology), and Shaylyn Kress (MA student, Dept. Psychology). The team performs presurgical functional MRI and white matter tractography (i.e., diffusion tensor imaging) in patients undergoing neurosurgery for various conditions, including temporal lobe epilepsy, tumours, cortical and vascular malformations, depression, obsessive-compulsive disorder, and other lesions. The goal is to localize eloquent cortex (i.e., cortex that, if removed, will result in loss of sensory, language, or motor function) adjacent to brain lesions in order to inform planning and decision-making for the surgery. Given that each patient presents unique challenges with respect to developing cognitive tasks that will activate regions near their surgical margins, the work involves designing individualized fMRI paradigms on a case-by-case basis to suit each patient’s specific needs. Since the formation of the team in 2013, the team has performed +200 presurgical scans. From these cases, several articles have been published including case reports, case series, and larger group studies. The team is also among the first to map the cranial nerves using tractography for posterior fossa tumours.
Dr. Layla Gould’s research also involves collaboration with Dr. Mike Kelly (Professor, Division of Neurosurgery) and Dr. Jon Farthing (Professor, Collage of Kinesiology) among other clinicians and researchers in the College of Kinesiology, Department of Neurology, and the Department of Physical Medicine and Rehabilitation on a project exploring a novel treatment (i.e., cross-education) for rehabilitation for patients with motor impairments following stroke. The study involves assessing strength and range of motion in stroke patients, as well as fMRI and tractography to examine the neural mechanisms associated with motor recovery post-stroke. The research will further reveal the translational implications of the cross-education effect in stroke rehabilitation.
