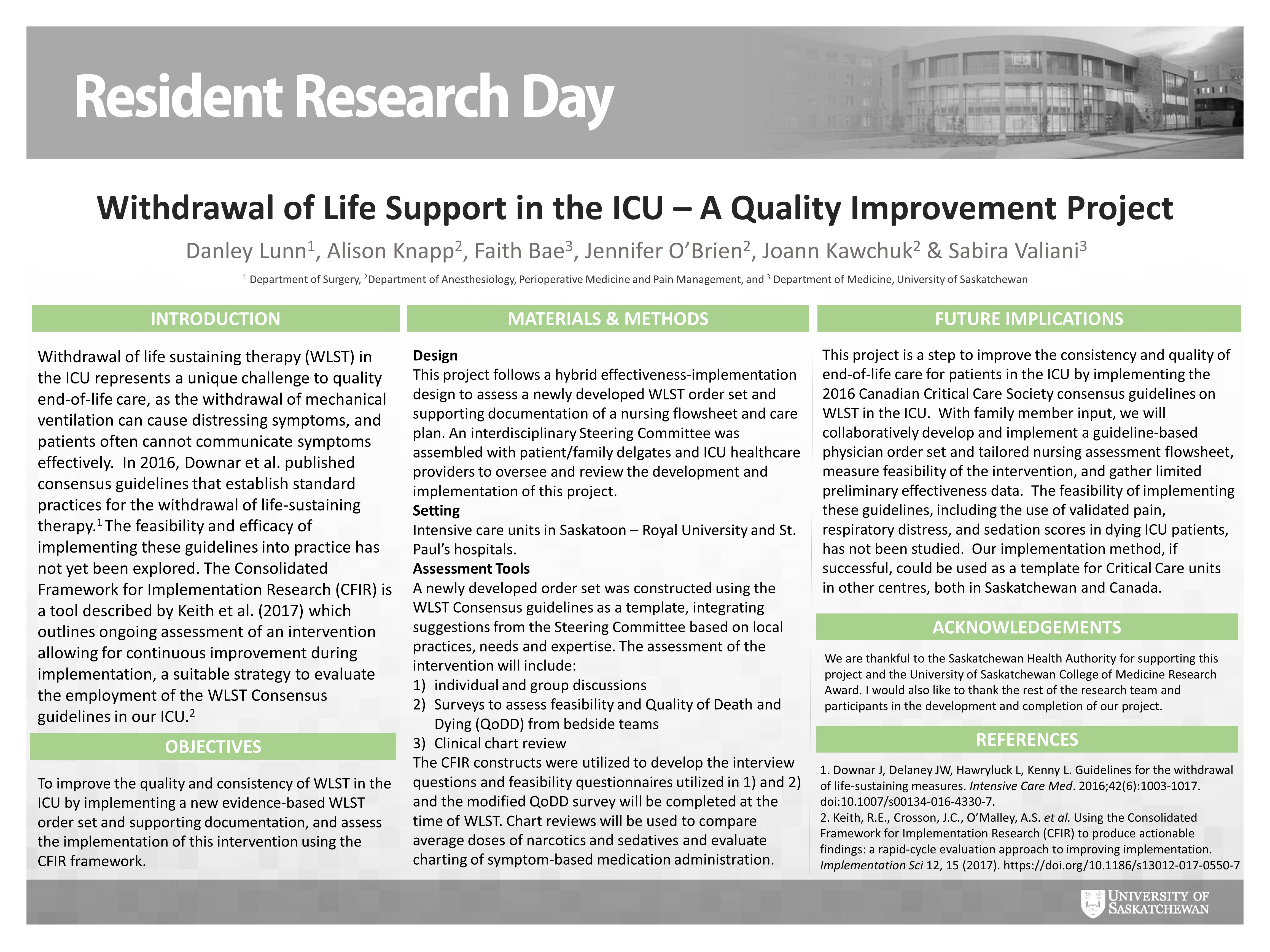
B2.0: Withdrawal of Life Sustaining Therapy in the ICU - a Quality Improvement Project
Danley Lunn, Alison Knapp, Faith Bae, Jennifer O’Brien, Joann Kawchuk, Sabira Valiani
Background: Withdrawal of life sustaining therapy (WLST) in the ICU represents a unique challenge to quality end-of-life care, as the withdrawal of mechanical ventilation can cause distressing symptoms, and patients often cannot communicate symptoms effectively. In 2016, Downar et al. published consensus guidelines that establish standard practices for the withdrawal of life-sustaining therapy. The feasibility and efficacy of implementing these guidelines into practice has not yet been explored. The Consolidated Framework for Implementation Research (CFIR) is a tool described by Keith et al. (2017) which outlines ongoing assessment of an intervention allowing for continuous improvement during implementation, a suitable strategy to evaluate the employment of the WLST Consensus guidelines in our ICU.
Purpose: To improve the quality and consistency of WLST in the ICU by implementing a new evidence-based WLST order set and supporting documentation, and assess the implementation of this intervention using the CFIR framework.
Methods: This project follows a hybrid effectiveness-implementation design to assess a newly developed WLST order set and supporting documentation of a nursing flowsheet and care plan. An interdisciplinary Steering Committee was assembled with patient family representatives and ICU healthcare providers to oversee and review the development and implementation of this project. The order set was constructed following the WLST Consensus guidelines as a template, and integrating suggestions from the Steering Committee based on local practices, needs and expertise. The assessment of the intervention will include 1) individual and group discussions 2) feasibility and Quality of Death and Dying (QoDD) surveys from bedside teams and 3) chart review. The CFIR constructs were utilized to develop the interview questions and feasibility questionnaires, the modified QoDD survey will be completed at the time of WLST and chart reviews will be used to compare average doses of narcotics and sedatives and evaluate charting of symptom-based medication administration.
