A2.0: Hypertensive crisis pre-catheter ablation for resistant atrial fibrillation: a case of undiagnosed bilateral pheochromocytomas
Nina Dhillon, Shravankumar Nosib
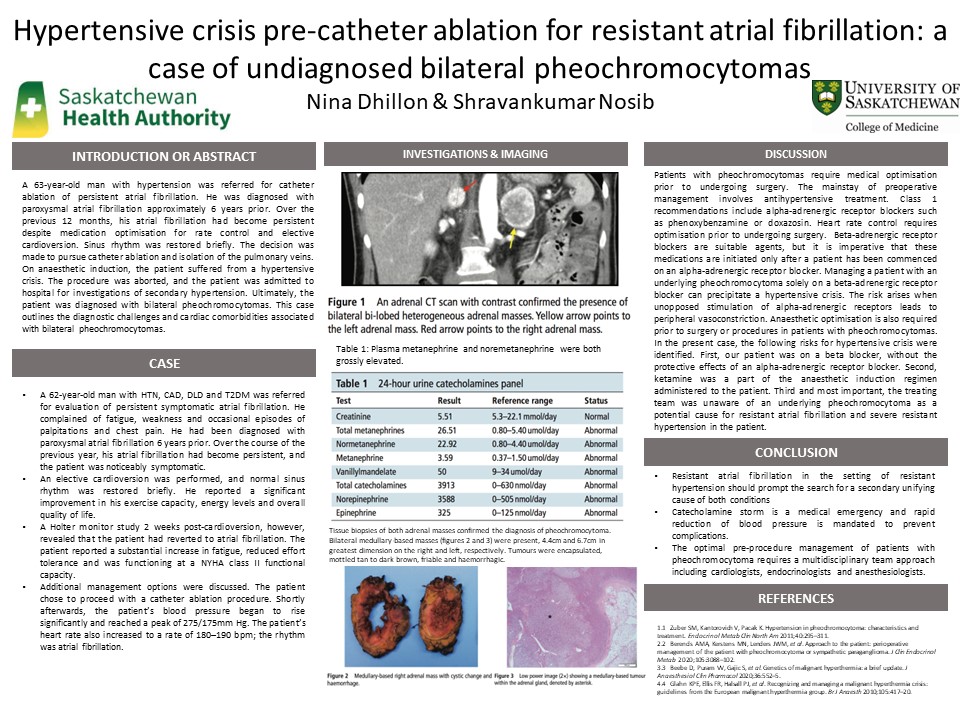
A 63-year-old man with hypertension was referred for catheter ablation of persistent atrial fibrillation. He was diagnosed with paroxysmal atrial fibrillation approximately 6 years prior. Over the previous 12 months, his atrial fibrillation had become persistent despite medication optimisation for rate control and elective cardioversion. Sinus rhythm was restored briefly. The decision was made to pursue catheter ablation and isolation of the pulmonary veins. On anaesthetic induction, the patient suffered from a hypertensive crisis. The procedure was aborted, and the patient was admitted to hospital for investigations of secondary hypertension. Ultimately, the patient was diagnosed with bilateral pheochromocytomas. This case outlines the diagnostic challenges and cardiac comorbidities associated with bilateral pheochromocytomas.
