Palliative Care Utilization Near the End of Life in Critically Ill Patients
Elizabeth Pywell
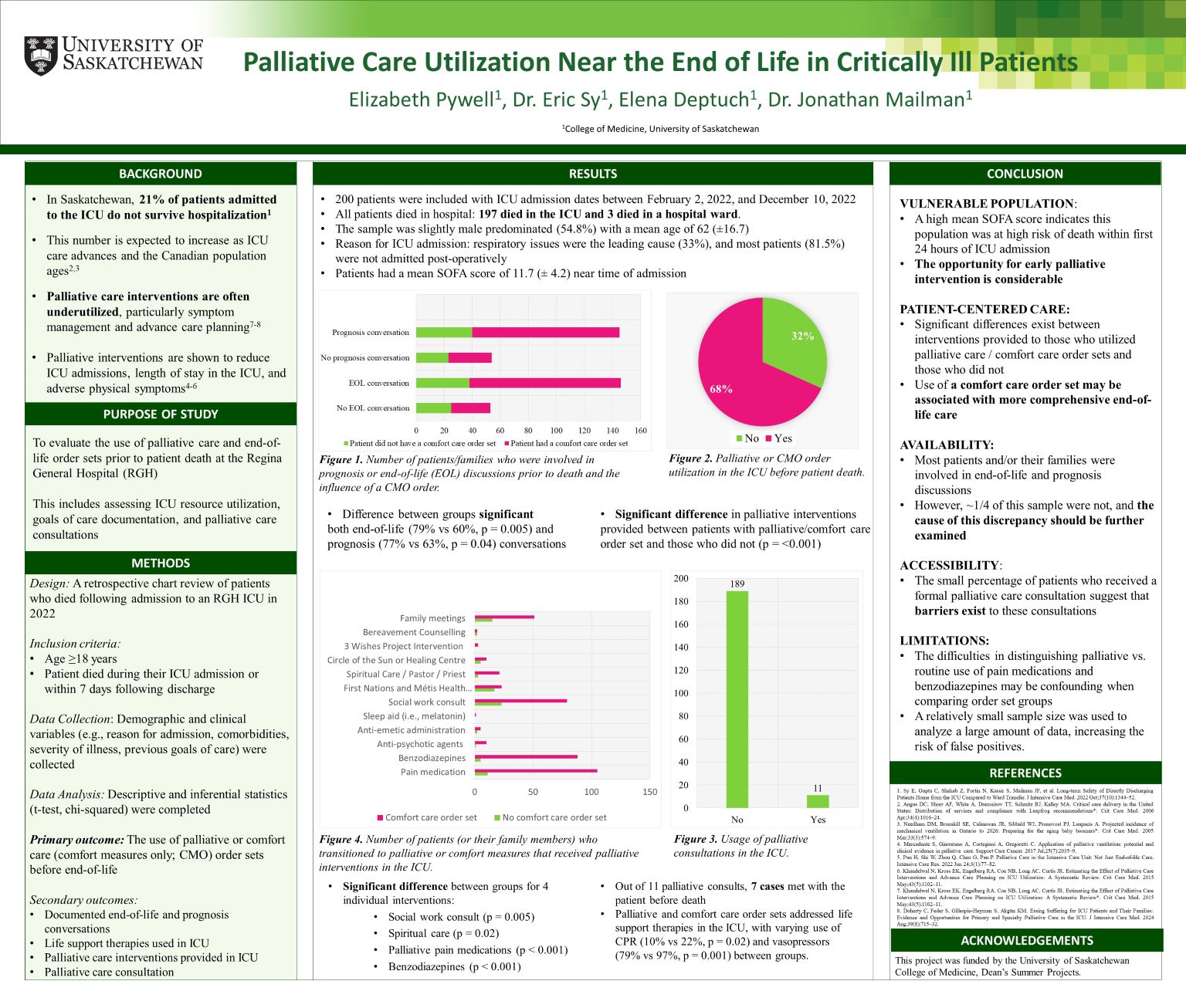
Palliative interventions can improve outcomes in the ICU; however, they are often underutilized. This study evaluates palliative care utilization in the ICU at Regina General Hospital to inform improvements in end-of-life care. A retrospective chart review included patients who died during their ICU admission or within 7 days and examined the use of palliative or comfort care order sets before end-of-life. Secondary outcomes included life support therapies and palliative care interventions provided, palliative care consultation, and documented end-of-life and prognosis conversations. The sample consisted of 200 patients with ICU admission dates between February 2 and December 10, 2022, with a mean age of 62, a slight male predominance (54.8%), and a mean SOFA score of 11.7 at admission. The results demonstrate that 68% of patients had a palliative or comfort care order set ordered before death, which was associated with increased utilization of palliative interventions, an increased likelihood of having a documented end-of-life or prognosis conversation, and decreased CPR and vasopressor use. Palliative care consultations occurred in only 11 (5.5%) of cases. These findings highlight the potential of palliative or comfort care order sets to improve end-of-life care and emphasize the need for improved palliative care integration in the ICU.
