Assessing the Impact of HIV Continuing Medical Education on Primary Care Clinical Practices in Saskatchewan
Rayan Shafi
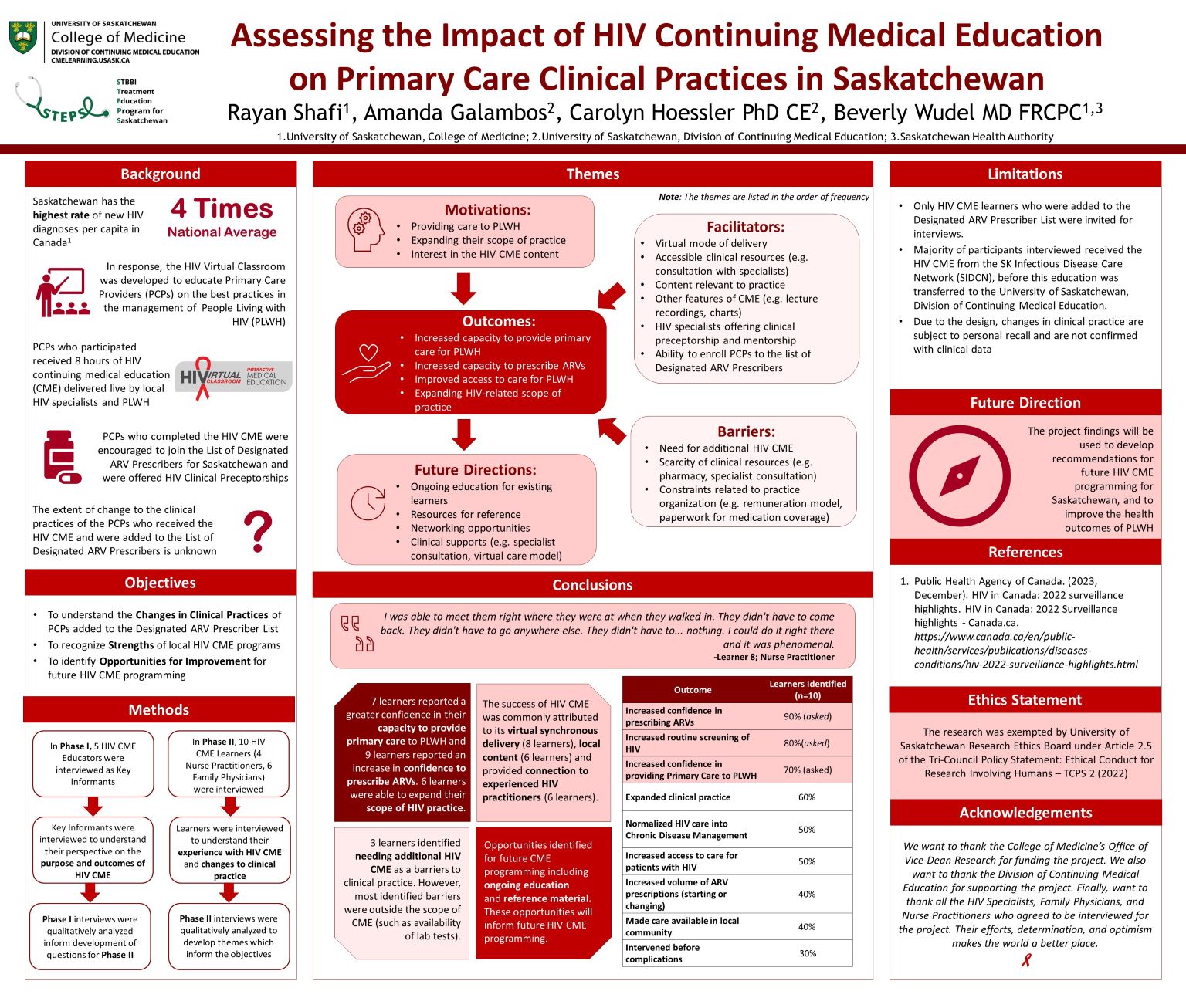
Background: Saskatchewan has the highest incidence of HIV diagnoses in Canada. HIV care has evolved and could be well-managed by Primary Care Providers (PCPs). HIV Continuing Medical Education (HIV CME) programming was created in Saskatchewan to empower PCPs to manage HIV and prescribe antiretroviral therapy (ART).
Methods: We assessed how HIV CME impacted PCPs’ clinical practices in Saskatchewan and their motivations and experiences. In Phase I, 5 HIV CME educator interviews were thematically analyzed to develop interview questions for Phase II. In Phase II, 10 HIV CME alumni were interviewed to understand motivations, outcomes, facilitators, barriers, and future education needs.
Results: Motivations included improving access to care and expanding scope of practice. Learner-reported outcomes included increased confidence in providing primary care, prescribing ART, and improved access to care for people living with HIV (PLWH). Facilitators included virtual delivery, preceptorship and mentorship. Barriers to changing clinical practice included a need for additional HIV CME, and scarcity of clinical resources. Ongoing education, quick reference materials, and HIV clinician networking opportunities were suggestions for future CME programming.
Conclusions: The PCPs reported increased confidence and improved access when providing primary care to PLWH and prescribing ART in the context of external clinical barriers to providing care.
