Sex Differences in In-Hospital Management and Outcomes of Patients with Acute Heart Failure
Amy Li
Acute heart failure (AHF) patients have high morbidity and mortality, yet sex-specific differences remain poorly understood. We conducted a retrospective chart review to investigate sex-based differences in clinical presentations and outcomes in 384 patients with AHF admitted to Regina General Hospital (2018 – 2023).
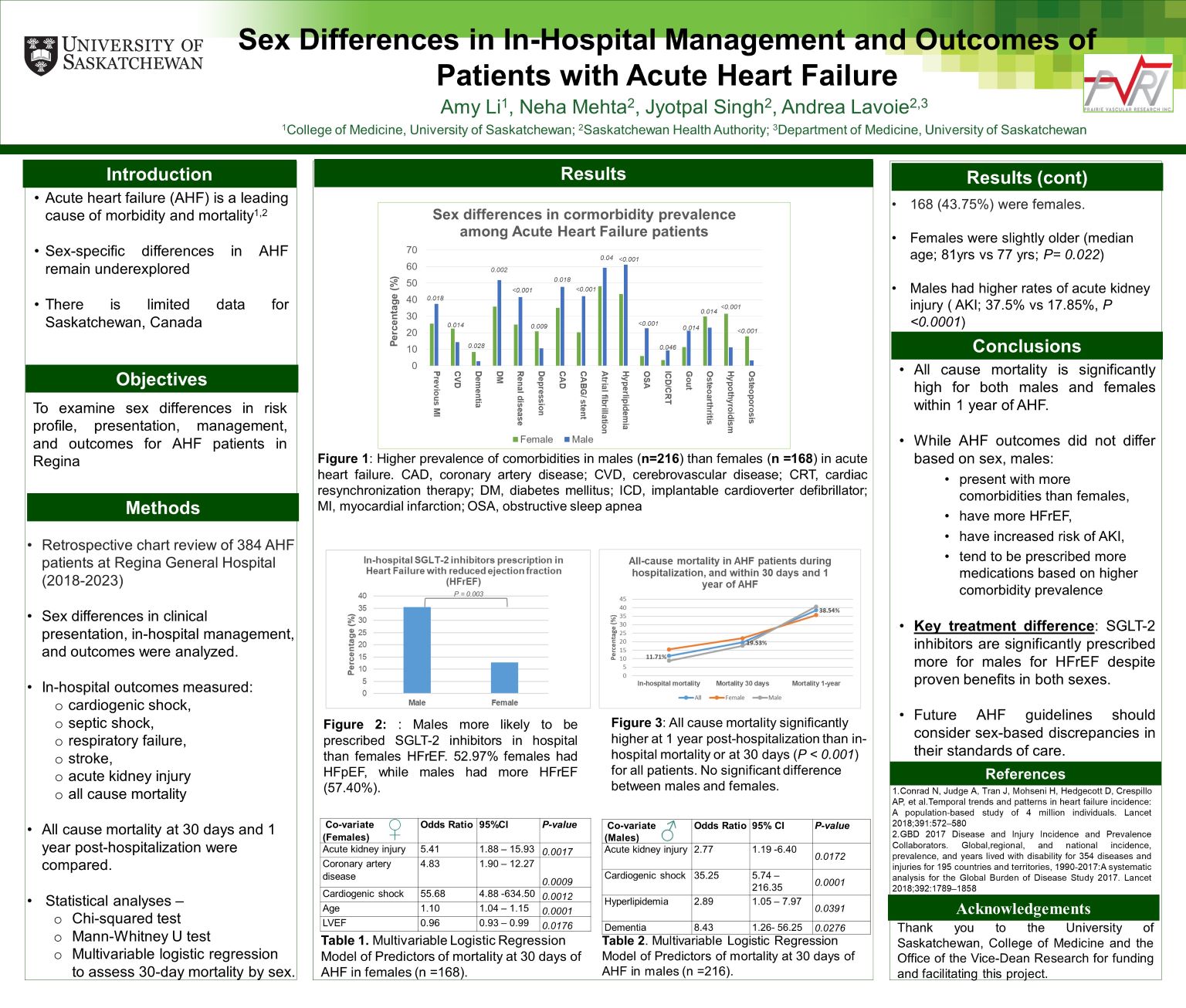
Among the 384 patients, 168 (43.75%) were women. Mortality at 1 year post-hospitalization (38.54%) was significantly higher than in-hospital mortality (11.71%) or mortality at 30 days (19.53%), although no sex-based differences were noted. Women more often presented with heart failure with preserved ejection fraction (HFpEF; 52.97%), while men had heart failure with reduced ejection fraction (HFrEF; 57.40%). Men presented with higher incidences of previous myocardial infarction, diabetes mellitus, renal disease, atrial fibrillation, coronary artery disease and hyperlipidemia. Men were more likely to develop in-hospital acute kidney injury and received more medications based on their comorbidities. SGLT-2 inhibitors were prescribed significantly more to men (35.48%) than women (12.72%) for HFrEF, regardless of being cornerstone heart failure therapy for both.
Despite similar mortality rates between sexes, men had more comorbidities and received more medications. SGLT2-inhibitors were found to be under prescribed in women despite their proven benefits. Future AHF guidelines should consider sex-based discrepancies in their standards of care.
