Anesthesia service provision in rural settings: a scoping review with findings mapped to the Core Outcome Measures for Perioperative and Anesthetic Care (COMPAC)
Muheeb Khan & Kyle Carriere
Background: Anesthesia provision in rural Canada faces challenges due to a shortage of qualified healthcare professionals, impacting patient safety and equity, with additional burdens on rural patients.
Objectives: This study aimed to identify anesthesia service models in rural areas and align these findings with a Core Outcome Set for anesthesia to identify knowledge gaps.
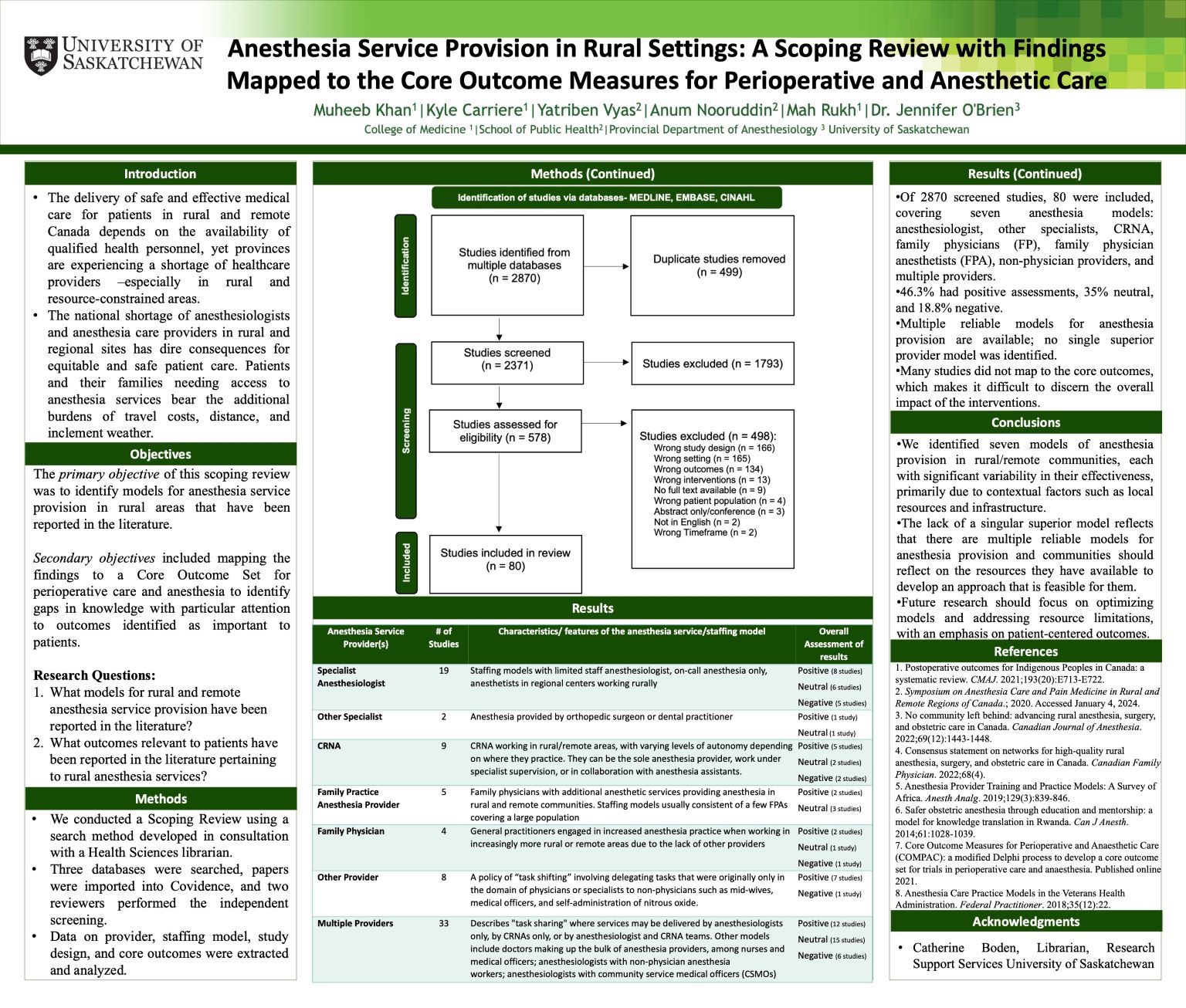
Design: We conducted a Scoping Review using a search developed in consultation with a Health Sciences librarian. We searched three databases, imported papers into Covidence, and two reviewers performed independent screening. Data on provider, staffing model, study design, and core outcomes were extracted and analyzed.
Results: Of 2870 studies screened, 80 were included, detailing seven anesthesia models: anesthesiologists, other specialists, CRNA, family physicians (FP), family physician anesthetists (FPA), non-physician providers, and multiple providers. 46.3% had positive assessments, 35% neutral, and 18.8% negative. No model was universally superior; effectiveness depended on local resources and infrastructure.
Conclusions: Multiple models for anesthesia in rural settings exist, but their effectiveness varies with local conditions. Communities should leverage available resources to develop tailored approaches that are most likely to work for them. Future research should focus on optimizing models and addressing resource and support gaps, with an emphasis on patient-centered outcomes.
