Utilization of in silico analysis for prediction of graft failure in kidney transplant
Eric Wang
Background: In kidney transplantation, HLA epitope mismatch based on high resolution HLA sequencing provides an advantage for risk stratification. We had analysed HLA surface epitopes to evaluate immunological compatibility between donors and recipients. Now, we explore how T-cell epitopes, and the indirect pathway are involved in graft rejection.
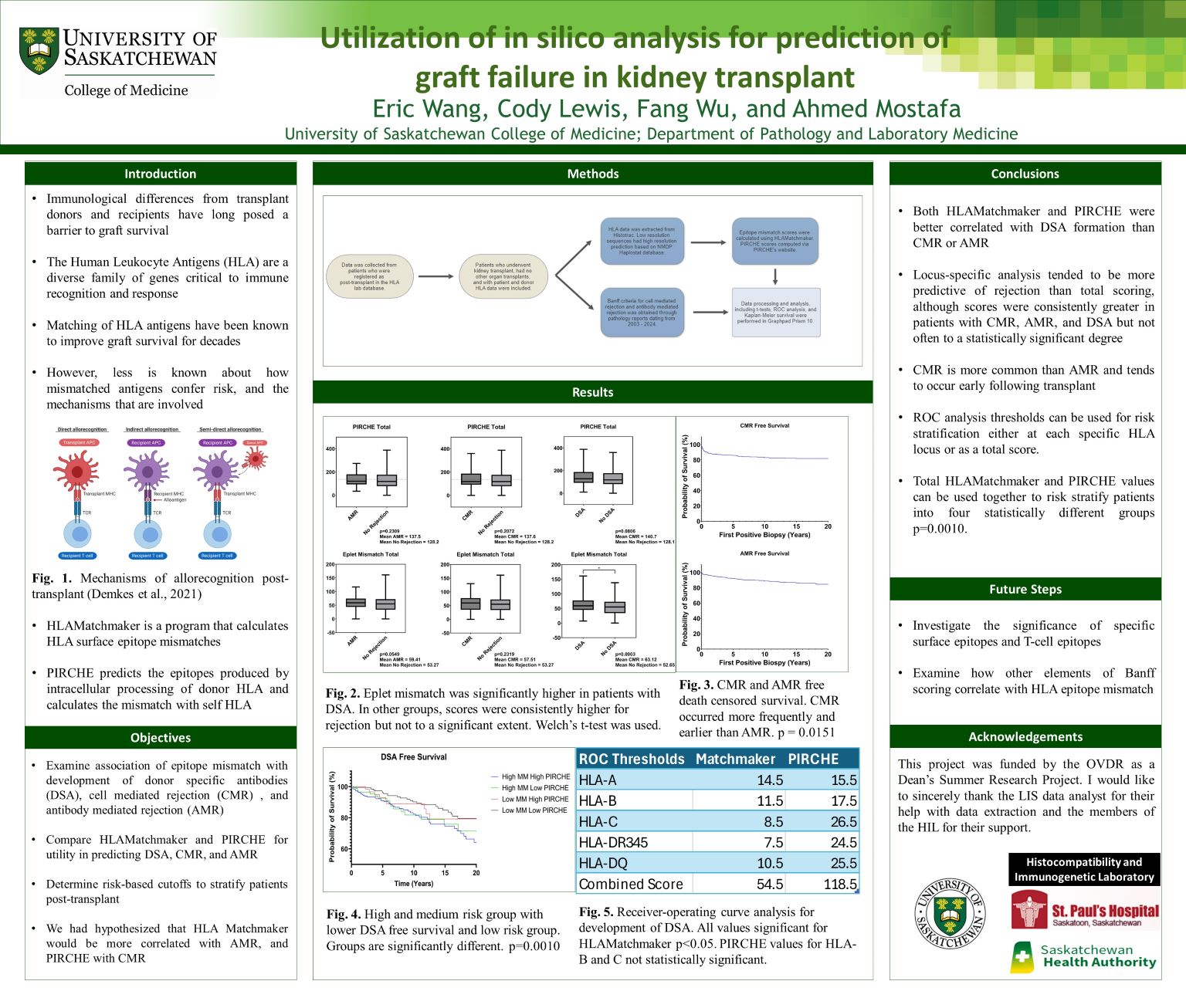
Methods: We obtained HLA and pathology data from 613 patients followed post renal transplant in Saskatchewan. Analysis for mismatch scores were calculated through HLAMatchmaker and PIRCHE. Banff criteria were extracted from renal biopsy reports.
Results: Overall and locus specific HLAMatchmaker and PIRCHE scores are correlated with DSA formation (p=0.003). CMR is more common than AMR (p=0.0151) and tends to occur earlier following transplant. Significant risk cutoff for Matchmaker scores were found at the following loci: A=14.5, B=11.5, C=8.5, DR345=7.5, DQ=10.5 and total 54.5 (p<0.05). PIRCHE values were significant for the following: A=15.5, DR345=24.5, DQ=25.5, and total 118.5 (p<0.05). DSA free survival showed significant difference between stratified groups (p<0.0010).
Conclusion: HLA epitope analysis is more predictive of DSA formation than for CMR or AMR. However, patients who developed CMR, AMR, and DSA consistently had higher scores for both HLAMatchmaker and PIRCHE. Overall, there are valuable clinical applications for epitope-based analysis post-transplant with multiple immune recognition pathways playing a role.
