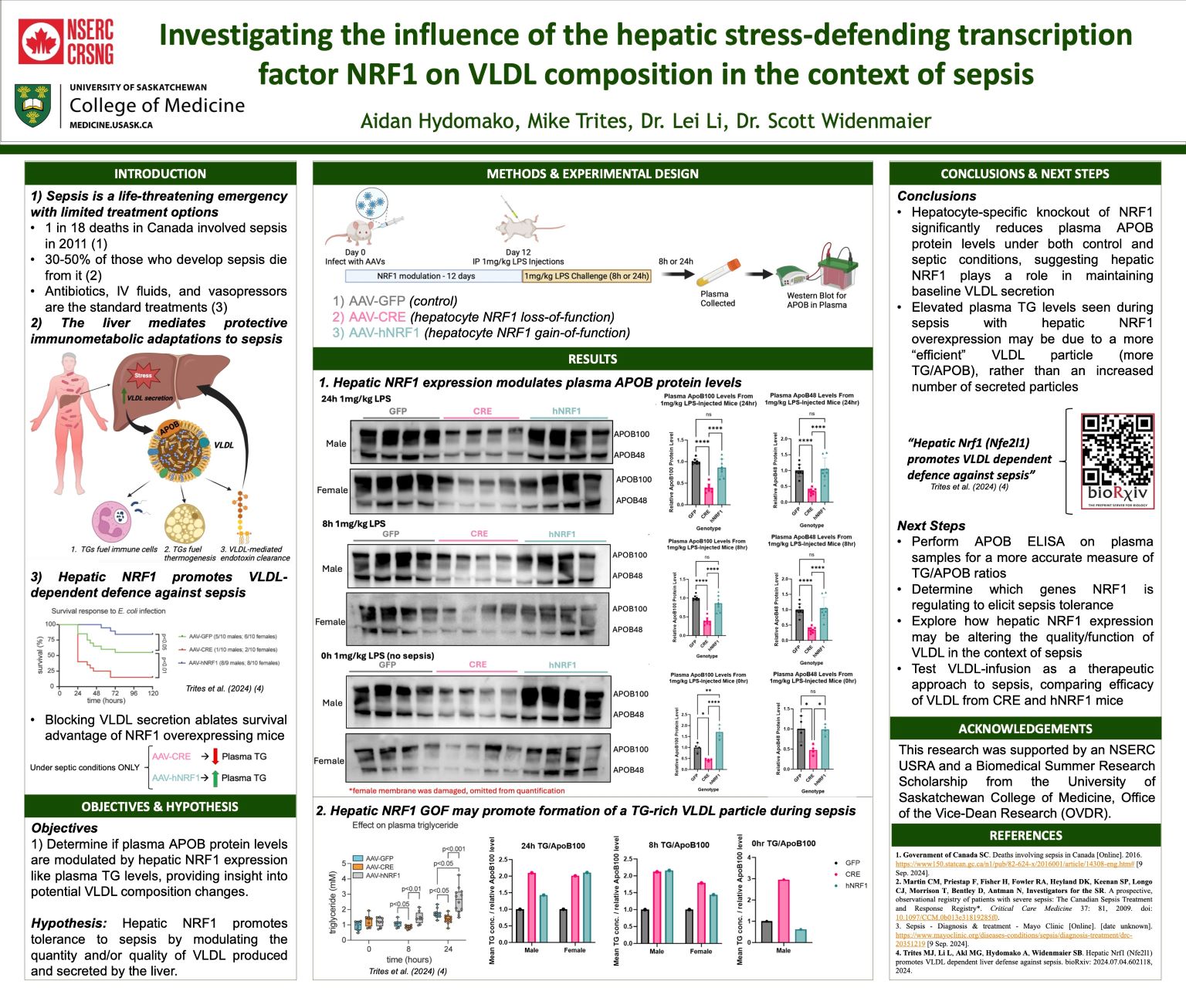
Investigating the influence of the hepatic stress-defending transcription factor NRF1 on VLDL composition in the context of sepsis
Aidan Hydomako
Sepsis is a life-threatening condition marked by a dysregulated immune response to infection, leading to acute inflammation, tissue damage, and multi-organ dysfunction. The liver mediates immunometabolic adaptations that promote survival during sepsis. Notably, infection and inflammation stimulate increased VLDL secretion by the liver, causing hypertriglyceridemia and supplying abundant lipids for immune cells and thermogenic tissues. We previously demonstrated that the hepatocyte stress-defence transcription factor NRF1 enhances sepsis tolerance by increasing VLDL secretion. Hepatic NRF1 deficiency in mice led to relative hypotriglyceridemia, hypothermia, and increased mortality. Conversely, overexpression promoted relative hypertriglyceridemia, prevented hypothermia, and improved survival. Here, we investigated the influence of hepatic NRF1 gain and loss of function on plasma APOB levels, the primary apolipoprotein on VLDL, during lipopolysaccharide-induced sepsis. We found that hepatocyte-specific NRF1 knockout reduces plasma APOB levels under both control and septic conditions, suggesting NRF1 plays a role in maintaining baseline VLDL secretion. Additionally, relative plasma APOB levels in NRF1-overexpressing mice were comparable to controls under septic conditions, despite elevated plasma triglycerides, suggesting that hepatic NRF1 promotes the formation of triglyceride-rich VLDL particles. Further investigation into hepatic NRF1-mediated tolerance mechanisms could reveal novel therapeutic approaches to addressing the global health burden of sepsis.
