Zapping brain cancer with long needles opens door to new treatments: USask research
SASKATOON – University of Saskatchewan (USask) researchers have developed a new method of killing brain cancer cells while preserving the delicate tissue around it. The technique also has a remarkable side-benefit: making chemotherapy treatment of brain cancer suddenly possible.
The technique involves placing long needles through the skull and sending pulses of electrical current into a glioblastoma tumour—the pernicious variety of brain cancer that caused Tragically Hip frontman Gord Downie’s death.
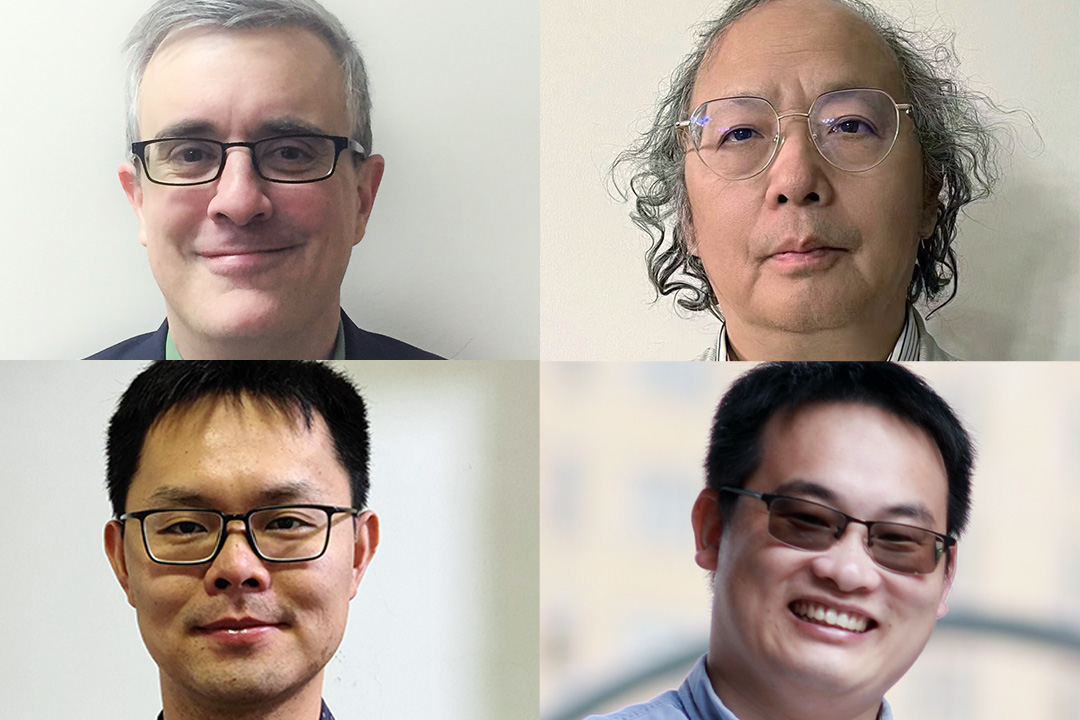
“A safer and more effective cancer treatment may be clinically possible,” said Dr. Mike Moser (MD), USask College of Medicine general surgery researcher and co-author of a study published recently in the Journal of Biomechanical Engineering.
“Patients with brain tumours may now have another option for local treatment that does not involve opening the skull, and does not involve heat or radiation.”
The USask-led research team created 3D models of cells to test which treatment protocols of electrical current—called irreversible electroporation (IRE or NanoKnife) and high-frequency irreversible electroporation (H-FIRE)—can destroy glioblastoma cells while minimizing the risk to surrounding tissues and blood vessels.
Glioblastoma, the most aggressive and deadly form of brain cancer, affects one in 25,000 Canadians, and only six per cent of those with the cancer currently survive longer than five years after diagnosis.
The technique relies on how glioblastoma cells respond to the electrical current. The researchers discovered tumour cells can be killed with a smaller electrical field than would kill surrounding healthy tissues.
They also discovered that this technique temporarily disrupts the blood-brain-barrier—the semi-permeable membrane that allows only tiny molecules to pass from the blood into the brain.
“The blood-brain barrier prevents many treatment drugs from getting to the tumour,” said USask biomedical engineering researcher Dr. Chris Zhang (PhD), co-author on the study. “We’ve shown that our technique can also help to open this barrier, so the brain is better able to receive other treatments—like chemotherapy or drugs that help increase the immune response—and help the patient fight the tumour in a systematic manner.”
The team also involved USask doctoral student Lujia Ding, and post-doctoral fellow Dr. Zheng Feng (PhD), as well as researchers from China’s Fudan University and Shanghai University. The project is part of an extended collaboration with Dr. Bing Zhang (PhD), a former USask doctoral student of Moser and Zhang.
The research was funded by CREATE and Discovery Grants from Canada’s Natural Sciences and Engineering Research Council, a grant from the Royal University Hospital Foundation, and a grant from National Natural Science Foundation of China to Dr. Bing Zhang and his team.
The next step in the research is to develop a combined method of tumour removal and immunotherapy using their H-FIRE technique.
-30-
For media inquiries, contact:Victoria Dinh
USask Media Relations
306-966-5487
victoria.dinh@usask.ca
Article re-posted on .
View original article.
