Interprofessional project tackles digital assessments
A pilot project is using the telehealth system to help assess chronic back pain in rural and remote Saskatchewan
By Marg SheridanA two-year old pilot study in rural Saskatchewan is getting technical – or at least digital.
The project, ‘Advancing interprofessional primary healthcare services in rural settings for people with chronic low back disorders,’ tackles a problem that a lot of health care specialties experience in the province: how do we provide better care and accessibility for those patients outside the big urban centres?
“We know that people in rural and remote communities have a higher likelihood of back pain and disorders compared to urban dwellers,” explained Dr. Brenna Bath, an assistant professor in the School of Physical Therapy and the Canadian Centre for Health and Safety in Agriculture (CCHSA), who is one of the lead researchers on the project. “We knew (from our clinical experience) that a lot of people were coming from rural and remote areas, and we were sending them back into the communities that didn’t necessarily have great access to care.
“People were sometimes travelling several hours, up to eight hours, to come for a one-hour back pain assessment.”
It’s not necessarily a new problem; in fact, it’s one that large countries like Canada often struggle with – how do we provide adequate care when some of our more at-risk populations live in remote areas? But as far as Bath knows, this is the first time that a project has looked at tackling physical therapy for back pain using a team approach through a videoconferencing lens.
So when the team was given an establishment grant by the Saskatchewan Health Research Foundation (SHRF) they started to implement the teleconference-side of the project with their partners at Kelsey Trail Health Region in central-eastern Saskatchewan.
“Our initial intent with the original grant was to join in with eHealth Saskatchewan’s telehealth network, and use telehealth compatible units,” Bath continued. “But because of a number of factors we weren’t able to get rolling with that technology as soon as we had hoped. Luckily for us eHealth Saskatchewan was piloting a new laptop-based secure system, and we were provided with access to that system, so we shifted our technology.”

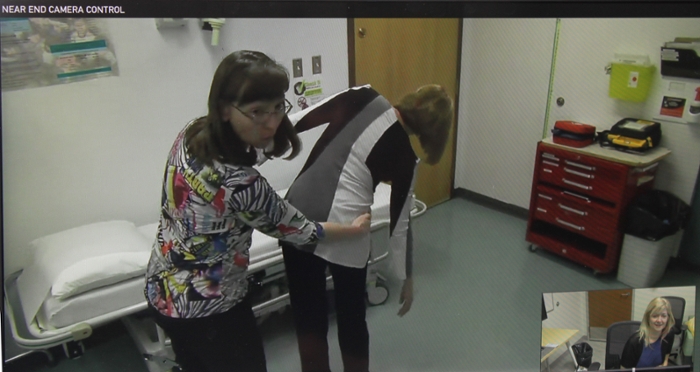
On one end of the technology is the patient and a nurse practitioner who acts as the ‘hands’ for the assessment, and on the other is a physical therapist, like Stacey Lovo-Grona, who gathers the patient history, directs the physical examination, and helps the team to come up with a management plan for the patient.
“With spinal assessment, however, the history is a very crucial part of diagnosing the problem, but the obvious major challenge (is) not being able to put your hands on the person to do a physical exam,” Lovo-Grona explained. “None of the telehealth literature for musculoskeletal problems examines an interprofessional model of care, so we began with team-building and training with the nurse practitioners to design an interprofessional back assessment whereby the nurse practitioner did the hands-on tests, and the physical therapist was the consultant.
“So this is quite an innovative approach to back pain assessment and management, and to our knowledge there’s nothing like it out there - we’re calling it a ‘teams and technology’ approach.”
The nurse practitioners have played a very significant role. While the grant has allowed Bath’s team to help pay for the nurses’ time and some additional training, their role is significantly closer to research partner than it has been employee. In fact, Bath and her team have found that they’re learning as much from the nurses as the other way around.
“Even though I’ve practiced spinal triage for ten years, this was a very special experience to be with a nurse practitioner,” Lovo-Grona stressed. “Nurse practitioners have extensive training and experience in chronic disease management as well as their history and rapport with the patients, it was a very valuable experience.”
In other words, what the team may have seen as a barrier before the project started has, in fact, become an area where they expect to see some fascinating qualitative information appear.
While the research is not yet complete, it looks promising that this new approach to both using telehealth as a clinical tool, and videoconferencing assessments with physical therapists can dramatically increase the access to physical therapy services for rural and remote Saskatchewanians.
As Bath explains, it’s a first for telehealth as well.
“We’re now running another small pilot using the telehealth network and compatible technology, and are the first group at the University of Saskatchewan that has a designated telehealth unit outside of the health region for clinical purposes.”
The new project is part of a Master’s of Physical Therapy student research group, funded by the College of Medicine.
