A different approach to teaching
The new Royal College 'Competence by Design' curriculum is hoping to put the onus on a milestone-based education
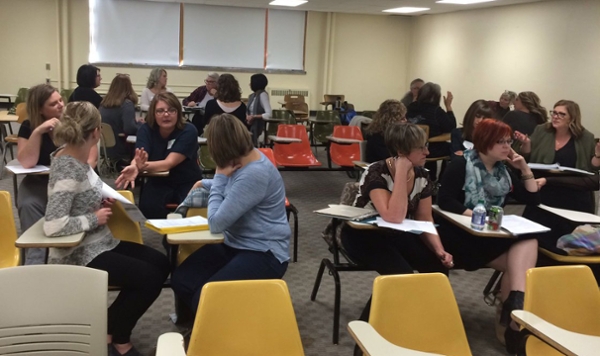
By Marg SheridanA Saturday morning isn’t usually when you’d expect to find faculty, staff, administrators and residents gathered together in the 1150 Health Sciences auditorium.
But in early November that’s exactly where they all were – coffees in-hand, and settling in for a day of presentations and workshops led by the Royal College of Physicians and Surgeons of Canada about the new Competence by Design (CBD) curriculum.
“I think we’ve got a good education system, but there are some gaps in the output of our graduates,” Dr. Ken Harris, the executive director of the RCPSC’s Office of Education, explained regarding the need for a new educational model. “(But) with so much of the training taking place in large academic centres sometimes people feel ill-prepared to enter directly into practice in smaller towns, or don’t have the skills to go on to a more in-depth, focused research-based practice.
“Sometimes we create things that might work in downtown Toronto, or other very large centres, but in fact don’t work for some smaller schools.”
It also means that there are times when the prescribed education model means that the trainees can sometimes become so involved with their ward-work that they may develop gaps in their outpatient skills.
“If you take that and distil it into the fact that every student is different, (it shows) we need a system where individuals can get these learning experiences and gain these competencies,” Harris continued. “Not so much by putting the time in in a block rotation as demonstrating their performance through a variety of things.”
What CBD boils down to is a different approach to giving residents the education they’ll need once they’ve left the college by changing from a timed, module rotation approach where teachers have to teach a learner to the best of their abilities in a given timeframe, into one that’s more milestone-based.
“So not just the things they need to know, but what they have to actually do,” stressed Dr. Sharon Card, who is helping to guide the division of general internal medicine through the change. “The intent is to provide a scaffolding where faculty can provide more targeted, quality feedback.”
She uses children’s soccer as an analogy for the change – if you watch kids get promoted from Timbit soccer through to a more club-like setting, they move up based on hitting skill milestones.
“We’ve tried to go back and actually look and see where we’re currently not preparing graduates as well as we could and where are the current needs of the public, and try to make that much more explicit,” Card continued. “It should make it easier for the learners to see what they actually need to achieve to make sure they can do what they need to do out in practice, so not just the things they need to know, but what they have to actually do.
“A curriculum (that) can then be prepared around needs of the future practice environment.”
And while Card foresees a slight uptick in the work the faculty may need to do during the initial transition, in the long run the expectation is that it will mean both less work for the faculty, and a more practice-prepared resident.
And that, in turn, will help the CoM.
“I think it’s going to add a lot of flexibility for the individual schools in how they develop the curriculum,” Harris stressed. “So it could help the schools to develop a particular focus, or how they develop a particular niche.
“And I think that’s great because every school is different.”
For more information on CBD, visit the Royal College website.
