Medical Imaging is a department of the College of Medicine. It also is an integral element of the Saskatchewan Health Authority.
We focus on two major goals:
- providing medical imaging services; and
- training radiology residents.
We also participate in training opportunities for medical, dental, nursing, technology and postgraduate learners. A broad range of research activities are also being pursued by faculty, postgraduate students and residents.
The Department of Medical Imaging Services within Saskatchewan Health Authority is committed to improving the healthcare of patients by providing excellence in diagnostic imaging and treatment.
We are dedicated in setting standards of excellence of radiological care and training of personnel including residents, appropriateness criteria, clinical and imaging protocols, and outcome expectations.
We promote scientific inquiry among its members for the advancement of imaging through clinical research, basic biomedical research and technology assessment, and clinical practice guidelines and outcomes research.
Our goals are that its members provide comprehensive diagnostic imaging by the most appropriate radiological evaluation and thus deliver the highest professional quality of care with optimal patient outcomes.
Undergraduate Medical Education Program
The Department of Medical Imaging has a key role in the delivery of the undergraduate medical education (UGME) program in the University of Saskatchewan’s College of Medicine.
The department is committed to supporting medical students in gaining foundational knowledge and skills related to medical imaging which they can draw upon regardless of what area of medicine they will practice in the future.
Faculty in the department provide lectures across the pre-clerkship and clerkship medical education curriculum, facilitate small group clinical sessions with medical students, and supervise students pursuing a clinical elective in Diagnostic Radiology. The department also welcomes pre-clerkship medical students who wish to shadow radiologists in the department.
Electives
A two-week elective in Diagnostic Radiology is available to final year medical students with exposure to all facets of the specialty. The goal of this elective is to develop a better understanding of Diagnostic Radiology as a medical specialty through exposure to the major imaging modalities in the department, by observing the imaging workflow and attending rounds, and through self-directed learning.
Students will be scheduled to a range of imaging modalities and will work with various radiologists and residents in Saskatoon or Regina. Students will be provided time for independent learning and access to an online course developed by the department. Students are also encouraged to attend the academic half-day teaching sessions for the residents held every Wednesday or Friday afternoon at Royal University Hospital.
Students will participate in assigned reading, pre-tests, and post-tests. Assessment will be based on a pre-test and post-test, and faculty and resident evaluations.
Electives are available to University of Saskatchewan students and out-of-province students.
Thank you for your interest in our department and our specialty.
UGME Program Contacts
Dr. Scott Adams
Departmental UGME Program Director
UGME Program Administrator
Residency Program
The University of Saskatchewan Training Program in Medical Imaging is designed to provide the best possible training in all aspects of imaging. The program is an intensive one, with considerable emphasis on teaching, in addition to exposure to a large volume of clinical pathology. The university-wide integration and rotational system ensures that each resident will have access to all the strengths of our faculty and clinical pathology. Residents have the opportunity to train at modern hospitals. All hospitals are equipped with state-of-the-art equipment including CT, MR, biplane angiography, and PET/CT at Royal University Hospital. Residents work daily with the best of general radiographic, ultrasound, CT and MRI technology. All hospitals have digital image archiving and communication systems.
The five year program consists of one year of preliminary clinical training (PGY1), followed by four years of training in medical imaging. All residents must be knowledgeable about the physics of medical imaging. To that end, intensive instruction is provided in each of the PGY2 and PGY3 years.
For more information, please visit the CaRMS website or contact Amanda O'Leary Senior Program Administrative Assistant (Resident and Medical Students) or Kailey Friesen Program Administrative Assistant
Log in to Sharepoint with nsid and password. Restricted for Faculty and Residents of Diagnostic Radiology only.
The program director is the head of the residency training committee. There are two resident representatives on the committee along with representatives from all the training sites in Saskatoon. This committee meets formally quarterly. More urgent topics are discussed on an as needed basis.
There is a yearly day-long retreat for all residents (PGY1-5) with the program director. Other speakers/attendees are invited as needed.
PGY-1
The PGY-1 year represents a broad clinical experience including a four week introduction to medical imaging. The current rotations include: ER, pathology, obstetrics, pediatrics, medicine and surgery. Two one-month elective blocks are also included.
PGY-2 to 5
A rotation schedule is established that satisfies the requirements of the Royal College of Physicians & Surgeons of Canada in regards to the content of training. The program emphasizes providing sound training in general diagnostic radiology. The different rotations are spread throughout the years of the program allowing the resident to gain graded responsibility in each area as well as taking on an increasing consultative role.
American Institute for Radiologic Pathology (AIRP)
Elective attendance at AIRP is encouraged and will be financially supported. Elective experiences are also available at affiliated sites in Saskatoon, and Regina. This offers an opportunity to experience radiology outside of a tertiary care centers.
An academic half-day program is offered weekly September-June. There is a formal series of 4hour weekly lectures or seminars for all residents, PGY1-5. Additional case-bases session occur weekly at the RUH site and about once or twice a month at the other sites in Saskatoon.
Interdisciplinary rounds occur with orthopedics, rheumatology, neurosurgery, neurology, oncology, head and neck surgery and respiratory medicine at various times during the month.
Journal Club meetings are organized by the residents and occur once a month.
The residents are expected to undertake two complete research projects during their five years of their training. A broad range of types of projects can be performed, ranging from retrospective views through quality assurance, to prospective randomized clinical trials. It is expected that a question will be posed and subsequently answered through the process of research. If it is felt to be appropriate, presentation of materials at National or International conferences is supported by the department. Presentation at our local Resident Research Day is mandatory, but additional presentations are voluntary. The PGY-1 Residents attend the research day.
Residents can click here to Access a complete document for research training objectives and requirements.
All residents are evaluated continually with evaluation reports at the completion of each 4-week or 8-week block of training. These evaluations are summarized into compiled evaluation reports every 6-months, with formal promotion reports yearly.
Objective assessment occurs with the use of oral exams yearly for PGY2-4. The PGY5 trainees receive an intense series of personal exams geared for exam preparation.
All trainees (PGY2-5) participate in a yearly OSCE examination in the spring.
All trainees (PGY2-5) write the American College of Radiology in-service examination.
Research
The Royal College of Physicians and Surgeons of Canada (RCPSC) objectives of training and specialty requirements that pertain specifically to research highlight the need to be able to critically appraise sources of medical information, in order to appropriately integrate new information into clinical practice and to be able to contribute to or collaborate in the development of new knowledge in the field of Radiology. Specifically, the resident will be required to be familiar with the development, execution, data analysis, interpretation and presentation of a research project by active participation in at least one research project during residency training, to understand the basic principles of basic and applied clinical research, , and to be able to critically appraise and summarize the literature on a given subject, and judge whether a research project or publication is sound, ethical, unbiased and clinically valuable. CanMEDS requires that completion of these objectives in each residency programme be formally evaluated using In-Training Evaluation Reports (ITERs) and Final In-Training Evaluation Reports (FITERs).
The goal of developing these Resident Research Training Objectives was to standardize minimum resident research requirements in Canada. This document was developed through collaboration and consensus by all members of the Research Committee. The guidelines describe research requirements expected of all residents successfully completing residency training programs in Canada. The achievement of Level I is the standard requirement by a resident, while Level II may be achieved by some residents with interests in clinical, basic science or population health research. Time lines during residency to complete the different requirements are outlined.
Researchers must submit for research ethics approval (REB) and apply for operational approval. The operational approval requests are submitted to Shawna Weeks, for review, follow up and assignment of OA file number.
Signatories for all departments impacted by the research will receive copies of the necessary documents (ie: OA application, REB application, data collection tools, manuals, etc). For Medical Imaging and Nuclear Medicine, Christine Dawson is the signatory.
Research Grants from Residents and Faculty
University of Saskatchewan Department of Medical Imaging members’ names in bold
2017
Title: Saskatchewan Bone Strength Development Study
Agency: Canadian Institutes of Health Research
Principal Investigators: Kontulainen S, Nour M
Co-investigators: Wiebe S, Arnold B, Baxter-Jones, Cooper D, Johnston J, Lanovaz J, Muhajarine N, Szafron M, Vatanparast H, Wark J
Amount Awarded: $100,000.00
Duration: May 2017-2018
Title: Zirconium-89 target development, production and in vivo validation.
Agency: Fedoruk Centre
Principal Investigator: Humphrey Fonge
Amount Awarded: $215,625.00
Duration: January 2017 to December 2019
Title: Radiotherapy strategies to eliminate T cells latenly infected with HIV provirus.
Agency: Canadian Institutes of Health Research (CIHR)
Principal Investigator: Ivan Sadowski
Co-investigator: Humphrey Fonge
Amount Awarded: $250,000.00
Duration: January 2017 to June 2018
Title: Alpha particle labelled antibodies for targeted alpha therapy (TAT).
Agency: Atomic Energy Agency of Canada
Principal Investigator: Humphrey Fonge
Amount Awarded: $20,000.00
Duration: April 2015 to March 2017
Agency: Fedoruk Centre
Principal Investigator: Clarence R. Geyer
Co-Principal Investigator: Humphrey Fonge
Amount Awarded: $211,000.00
Duration: February 2015 to January 2017
2018
Title: Development and evaluation of a remote robotic ultrasound clinic model to improve access to medical imaging in northern and Indigenous communities.Agency: Saskatchewan Health Research Foundation and Saskatchewan Centre for Patient-Oriented Research.
Principal Investigator: Mendez I
Co-Principal Investigator: Burbridge B
Co-Investigator: Adams SJ, Babyn P, Stoneham G, Ramsden V, McKinney V, Penz E
Amount Awarded: $154,153
Duration: 2018-2020
Title: Targeting insulin growth factor receptor in Herceptin resistant breast cancer with novel alpha particle_labelled antibody drug radioconjugates.
Agency: Canadian Breast Cancer Foundation
Principal Investigator: Humphrey Fonge
Amount Awarded: $366,500.00
Duration: September 2015 to August 2018.
Title: Targeting non-responsive Her2-positive breast cancer with novel anti-Her3 alpha-particle labelled antibody drug radioconjugates.
Agency: Saskatchewan Health Research Foundation (SHRF)
Principal Investigator: Humphrey Fonge
Amount Awarded: $120,000.00
Duration: September 2015 to August 2018.
2019
Title: Improving lung cancer diagnosis with novel artificial intelligence imaging analytics.Agency: Saskatchewan Health Research Foundation and Saskatchewan Centre for Patient-Oriented Research.
Principal Investigators: Babyn P,
Co-investigators: Adams SJ, Burbridge B, Stoneham G, Mendez I, Penz E, Tyan C-C, Longo J, Zarzeczny A, Skrapek C, Belitski K
Amount Awarded: $179,686.00
Duration: 2019-2021.
Title: Production, processing and evaluation of pharmaceutical-grade 225Ac and 67Cu for cancer theranostics
Agency: Sylvia Fedoruk Centre, Operating Grant,
Principal Investigator: Humphrey Fonge
Co-investigators: Eric Price, Ekaterina Dadachova, Patrick Causey, Valery Radchenko
Amount Awarded: 165,000
Duration: 04/2019 to 03/2021
Title: Alpha particle-labeled antibody-drug radioconjugates for radiotherapy of metastatic colorectal cancer (mCRC)
Agency: Canadian Institute for Health Research (CIHR),
Principal Investigator: Humphrey Fonge
Co-investigators: Clarence R. Geyer
Amount Awarded: $872,100.00
Duration: 05/2019 – 04/2024
Title: Molecular imaging of prostate cancer using 68Ga-PSMA PET/CT – a clinical trial
Principal Investigator: VarunKumar Bathini
Co-principal investigators: Humphrey Fonge, Rajan Rakheja
Co-investigators: Clarence R. Geyer
Amount Awarded: $14,000.00
Duration: 05/2019 – 04/2020
Title: Non-clinical pharmacology with linac-produced pertechnetate
Agency (research contract): Canadian Isotope Innovation Corp
Principal Investigator: Humphrey Fonge
Amount awarded: $120,000.00
Duration: 01/2019 – 04/2020
Knowledge translation activities - Approved Clinical Trial Applications (CTA)
Health Canada approved CTA
Evaluation of 89Zr-DFO-nimotuzumab for non-invasive imaging of EGFR+ cancers by Positron Emission Tomography (PET)Approval ID: HC6-024-c219924
Principal Investigators: Rajan Rakheja MD, Vijay Kundapur MD, Tahir Abbas MD, Sundeep Nijjar MD, Almgrahi Abdulaziz MD, and Humphrey Fonge PhD.
Research Ethics Board approved CTA
Investigation of the Sensitivity and Specificity of 68Ga-HBED-CC-PSMA PET/CT in Prostate CancerApproval ID: REB ID: # 130
Principal Investigators: Rajan Rakheja MD, Varunkumar Bathini MD, Sundeep Nijjar MD, Almgrahi Abdulaziz MD, Nayyer Iqbal MD, Ali El-Gayed MD, Humphrey Fonge PhD.
Diagnosis of Parkinson’s disease and related disorder using [18F]FDOPA
Approval ID: REB ID: Bio # 18-56
Principal Investigators: Rajan Rakheja MD, Ali Rajput MD, Alex Rajput MD, Humphrey Fonge PhD.
Evaluation 89Zr-DFO-nimotuzumab for non-invasive imaging of EGFR-positive cancers by PET/CT.
Approval ID: REB ID: Bio-17-288
Principal Investigators: Rajan Rakheja MD, Vijay Kundapur MD, Tahir Abbas MD, Sundeep Nijjar MD, Almgrahi Abdulaziz MD, and Humphrey Fonge PhD.
- Haron Obaid – Promotion to Full Professor
- Kristin Atkinson – Graduated in Business Administration, Edwards School of Business, U of S
- Vice Dean Research Prize for Resident Research in Medical Imaging – Dr. Scott Adams, PGY-2
- Stuart Houston Award for Medical Imaging Research-Dr. Leanne Langford, PGY-2 “Determining Residual Gastric Volume in Healthy Children using Ultrasound”
- Honorable Mention: Dr. Scott Adams, PGY-2 | Project: “Patient Perspectives and Priorities Regarding Artificial Intelligence in Medical Imaging”
- Honorable Mention: Dr. Raza Naqvi, PGY-3 | Project: “Comparison of Surgical Intervention Rates for Knee MRI’s Ordered by General Practitioners and Orthopedic Surgeons”
- Best Practice Quality Improvement Award: Dr. Raza Naqvi, PGY-3 | Project: “The Effect of Coordinated Investigations for Rural Lung Cancer Patients on Traveling and Time to Staging Completion”
- Honorable Mention: Dr. Graeme Bell, PGY-3 | Project: “Implementation of a Tailored MRI Stroke Protocol”
- RSNA Roentgen Research Award: Dr. Scott Adams, PGY-2
- Best Non-Clinician Researcher Presentation Award: Una Goncin | Project: “Contrast-Enhanced Perfusion Imaging in Teloest Model Organisms, Rainbow Trout (Onchorhynchus mykiss)”
- Best Clinical Teacher of the year in Medical Imaging: Dr. Derek Fladeland and Dr. Jeffrey Bird
- Best Researcher of the year in Medical Imaging: Dr. Steven Machtaler
- 1st Place Tie CoMRAD Award Symposium-Dr. Scott Adams, PGY-2
- Canadian Radiological Foundation Leadership Scholarship, presented to Dr. Scott Adams, PGY-2.
2018
- Stuart Houston Award for Medical Imaging Research-Dr. Scott Adams, PGY-1 | Project: “A Crossover Comparison of Standard and Telerobotic Approaches to Prenatal Sonography”
- Honorable Mention: Dr. Neil Kalra, PGY-4 | Project: “Appropriateness in Residency Education: An Initiative in Medical Imaging to Promote System Resource Stewardship”
- Best Practice Quality Improvement Award – Dr. Raza Naqvi, PGY-2 | Project: “The Effect of Coordinated Investigations for Rural Lunch Cancer Patients on Traveling and Time to Staging Completion”
- Honorable Mention: Dr. Yan Du and Dr. Gage Watson | Project: “ Use of Oral Contrast in the Setting of Undifferentiated Abdominal Pain in the Emergency Room”
- Best Medical Student Project: Dr. Bjorn Hunter | Project: “Project Sympton Questionnaires Result in Higher ACR and CAR Appropriateness Scores Compared with Physician Requisitions for Knee MRI”
- Best Clinical Teacher of the year in Medical Imaging: Dr. Geoff Karjala
- Best Researcher of the year in Medical Imaging: Dr. Humphrey Fonge
- David Leswick – Promotion to Full Professor
- Kristin Atkinson – Completion of the Leadership Development Program, Edwards School of Business, U of S
2017
- Stuart Houston Award-Dr. Neil Kalra, PGY-3 | Project: “A Day in MR: Exam Variation and Appropriateness of MRI exams in Canada”
- Honorable Mention: Dr. James Huynh, PGY-5 and Dr. David Horne, PGY-5 | Project: “On Call Imaging at the University of Saskatchewan: An Assessment of Busyness Inter-Resident Variability (Call Karma)”
- Best Practice Quality Improvement award-Dr. Jimmy Wang, PGY-3 | Project: “On-line TI-RADS Calculator”
- Honorable Mention: Dr. Gage Watson, PGY-3 | Project: “Use of Oral Contrast in Setting of Undifferentiated Abdominal Pain in the Emergency Room”
- Best Medical Student Award – Jaques Van Heerden | Project: “The Utility of Dual Energy CT in Visualizing the Menisci in Patients Unfit for MRI”
- Honorable Mention: Evan Mah for his projects on Undergraduate Medical Training.
- CoMRAD Award Winners: Dr. Humphrey Fonge, Dr. Steven Machtaler and Dr. Haron Obaid
- Best Clinical Teacher of the year in Medical Imaging: Dr. Christina Theoret
- Best Researcher of the year in Medical Imaging: Dr. Brent Burbridge
- Sheldon Wiebe – Promotion to Full Professor
University of Saskatchewan Department of Medical Imaging members’ names in bold
2018
- Kanthan R, Baniak N, Adams S, Lee C-H, Chibbar R. Immunohistochemical and molecular characterization of extra-pelvic endometrial stroma sarcomas. XXXII Congress of the International Academy of Pathology, Dead Sea, Jordan, 2018.
- Yi X, Adams SJ, Babyn P, Elnajmi A. Automatic catheter detection in pediatric X-ray images using a scale-recurrent network and synthetic data. International Conference on Medical Imaging with Deep Learning, Amsterdam, 2018.
- Moulton KM. Imaging of Multiple Sclerosis, Demyelinating Diseases, and Important Mimics. MS Education Day (Invited Speaker). August 3rd, 2018. Saskatoon, SK.
- Moulton KM. Imaging in Acute Ischemic Stroke. Stroke Education Day (Invited Speaker). September 24, 2018. Yorkton, SK.
- Moulton KM. 4D CTA: Current Techniques and Applications. Neurosciences Grand Rounds (Invited Speaker). November 2nd, 2018. Saskatoon, SK.
- Adams S, Burbridge B, Mendez I, Babyn P. Assessment of a Telerobotic Approach for Prenatal Ultrasound Imaging. RSNA December 2, 2018, Oral Presentation.
- Alizadeh E, Solomon VR, Gonzalez C, Bernhard W, Makhlouf A, Barreto K, Geyer CR, Fonge H,. (2018). 89Zr-labeled domain II specific anti-EGFR ScFv-Fc antibody fragment for imaging and monitoring of response to anti-EGFR treatment by PET. Society of Nuclear Medicine Molecular Imaging, Philadelphia, United States
- P. Causey, D. Bureau, K. Leeder, R. Perron, S.V. Hartimath, H. Fonge. (2018). Production of a Thorium/ Actinium Generator at the Canadian Nuclear Laboratories. Society for Nuclear Medicine Molecular Imaging, Philadelphia, United States
2019
- Pike, S. Neonatal cranial ultrasound. Podium presentation. May 2019. SAMIM/SADMS annual conference.
- Sabri, Ali. Role of Breast Density in Risk & Detection Rate. April 2019. 35th Iranian Society of Radiology Conference.
- Sabri, Ali. Approach to Non Mass Enhancement in Breast MRI. April 2019. 35th Iranian Society of Radiology Conference.
- Sabri, Ali. I did the Biopsy, What is Next? Pathology Report Assessment by Radiologist. April 2019. Iranian Society of Radiology Conference.
- Sabri, Ali. Lung Cancer and Imaging, New Approach for Gene Positive Cancers. April 2019. Iranian Society of Radiology Conference.
- Naqvi S, Leswick D, Beavis C, Mondal P, Bryce R. Comparison of knee MRIs ordered by orthopedic surgeons and general practitioners. Canadian Association of Radiologists Annual Meeting, Montreal, QB 2019.
- Naqvi S, Bharadwaj S, Kennedy R, Bigsby R, Babyn P, Tyan C. The Effect of Coordinated Investigations for Rural Lung Cancer Patients on Traveling and Time to Staging Completion. American Thoracic Society Annual Conference, Dallas, TX, 2019.
- Burbridge B, Penz E, Wirth I, Naqvi S. The Clinical and Economic Impacts of Choosing a Diagnostic Imaging Examination – CT PE Case Study. Choosing Wisely Annual Conference, Saskatoon, SK, 2019 (date pending)
- Bell GDM, Moulton KM. Implementation of a tailored MR Stroke protocol. Canadian Association of Radiologists Annual Meeting, Montreal, 2019.
- Najafi Semnani A, Fotouhi R, Zhang Q, Obaid H, Adams S. Haptic force feedback for a teleoperated sonography system. (accepted for presentation at the 2019 Canadian Society for Mechanical Engineering International Congress, London ON)
- Adams SJ, Tang R, Henderson R, Babyn P. Patient perspectives and priorities regarding artificial intelligence in medical imaging. Canadian Association of Radiologists Annual Scientific Meeting, Montreal, 2019.
- Yi X, Adams SJ, Henderson R, Babyn P. Deep learning for automatic multi-catheter detection on pediatric radiographs. Canadian Association of Radiologists Annual Scientific Meeting, Montreal, 2019.
- Adams SJ, Burbridge B, Babyn P, Mendez I. Access to ultrasound imaging: Qualitative study in northern, remote Indigenous communities in Canada. Association of University Radiologists Annual Meeting, Baltimore, 2019.
- Adams SJ, Mendez I, Babyn P, Burbridge B. Long distance ultrasound imaging: Technical developments, clinical applications, and integration of telerobotic ultrasound systems into clinical practice. Association of University Radiologists Annual Meeting, Baltimore, 2019.
- Nguyen XV*, Adams SJ*, Hobbs S, Ganeshan D, Wasnik A. Radiologist as lifelong learner: Strategies for ongoing education. Association of University Radiologists Annual Meeting, Baltimore, 2019. *Co-presenters.
- Adams SJ, Hunter B, Babyn P. Demonstrating the value of artificial intelligence in medical imaging: Strategies for economic evaluation of artificial intelligence algorithms. Association of University Radiologists Annual Meeting, Baltimore, 2019.
- Bell G, Moulton KM. Implementation of a Tailored MR Stroke Protocol. Canadian Association of Radiologists Annual Scientific Meeting. April 11-14, 2019. Montreal, QC.
- Obaid, Haron. Advances in MRI Imaging of Sports Injuries. International Society in MR in Medicine (ISMRM). May 12, 2019. Montreal, OQ
- Solomon VR, Alizadeh E, Causey P, Makhlouf. A, Barreto K, Bernhard W, Wilson JJ, Geyer CR, Fonge H. (2019). Targeted alpha particle therapy of EGFR-positive breast cancer using site-specifically labeled 225Ac–dN-SpyCatcher-SpyTag-nimotuzumab. Targeted Alpha Therapy 11 (TAT11), Ottawa, Canada Conference
- Khan BAA, Causey P, Solomon VR, Bernhard W, Barreto K, Wilson JJ, Geyer CR, Fonge H. (2019). Biparatopic targeting of epidermal growth factor receptor positive breast cancer cells using domain I/II and domain III specific antibody conjugates. Targeted Alpha Therapy 11 (TAT11), Ottawa, Canada.
- Barreto K, Causey P, Solomon VR, Bernhard W, Sutherland A, Wilson JJ, Geyer CR, Sadowski I, Fonge H. (2019). Depleting the latent HIV-1 cell population using 225Ac-labeled anti-CD4+targeted radioimmunoconjugates. Targeted Alpha Therapy 11 (TAT11), Ottawa, Canada.
University of Saskatchewan Department of Medical Imaging members’ names in bold
2018
- Adams SJ, Burbridge B, Badea A, Kanigan N, Bustamante L, Babyn P, Mendez I. A crossover comparison of standard and telerobotic approaches to prenatal ultrasound imaging. J Ultrasound Med. 2018 Nov;37(11):2603-2612.
- Baniak N, Adams S, Chibbar R, Lee C-H, Kanthan R. Hepatic endometrial stromal sarcoma. Pathol Res Pract. 2018 Oct;214(10):1726-1731.
- Burbridge B, Adams S, Burbridge C. Computed tomography frequency and power injection utilization for a cohort of cancer patients with arm ports. J Rad Med Imag. 2018 Mar;1:1002.
- Adams SJ, Rakheja R, Bryce R, Babyn PS. Incidence and economic impact of incidental findings on 18F-FDG PET/CT imaging. Can Assoc Radiol J. 2018 Feb;69(1):63-70.
- Hernández-Ronquillo L, Adams SJ, Ballendine SA, Téllez-Zenteno JF. Epilepsy in an elderly population: classification, etiology and drug-resistance. Epilepsy Res. 2018 Feb;140:90-94.
- Adams SJ, Kirk A, Auer RN. Adult-onset leukoencephalopathy with axonal spheroids and pigmented glia (ALSP): Integrating the literature on hereditary diffuse leukoencephalopathy with spheroids (HDLS) and pigmentary orthochromatic leukodystrophy (POLD). J Clin Neurosci. 2018 Feb;48:42-49.
- Adams SJ, Burbridge BE, Badea A, Langford L, Vergara V, Bryce R, Bustamante L, Mendez IM, Babyn PS. Initial experience using a telerobotic ultrasound system for adult abdominal sonography. Can Assoc Radiol J. 2017 Aug;68(3):308-314.
- Wang, J., Ellchuk, T., Otani, R., Groot, G. and Babyn, P. (2018) Online TI-RADS Calculator. Open Journal of Radiology, 8, 175-180. doi: 10.4236/ojrad.2018.83020.
- Adams S, Burbridge B, Badea A, Kanigan N, Bustamante L, Babyn P, Mendez I. A Crossover Comparison of Standard and Telerobotic Approaches to Prenatal Ultrasound Imaging. Published online April 24, 2018, Journal of Ultrasound in Medicine 2018;37 (11): 2603-2612.https://doi.org/10.1002/jum.14619
- Burbridge B, Adams S, Burbridge C. Computed Tomography Utilization For a Cohort of Breast and Colon Cancer Patients with Arm Ports. J Radiol Med Imaging. 2018; 1: 1002. http://meddocsonline.org/journal-of-radiology-and-medical-imaging/Computed-tomography-frequency-and-power-injection-utilization-for-a-cohort-cancer-patients-with-arm-ports.pdf
- Vanderby Sonia, Badea Andreea, Pena-Sanchez Juan-Nicolas, Kalra Neil, Babyn Paul. A Day in the Life of MRI: The Variety and Appropriateness of Exams Being Performed in Canada. The Canadian Association of Radiologists Journal (CARJ). Volume 69(2); pg. 151-161. May 2018.
- Brent Burbridge, Chris Plewes, Grant Stoneham, Peter Szkup, Rob Otani, Paul Babyn, Rhonda Bryce. Randomized Clinical Trial Evaluating Complications and Complication-Related Removal of Arm-Situated Power-Injectable and Non-Power-Injectable Totally Implanted Venous Access Devices among Cancer Patients. J Vasc Interv Radiol. 2018 May; 29(5):648-656.
- Hadju I, Michel B, Al-Dulaymi M, Wasan K, Fonge H*, Badea I* (2018). A 89Zrlabeled lipoplex nanosystem for image-guided gene delivery: design, evaluation of in vitro stability and in vivo behaviour. Int J Nanomedicine. 2018 Nov 21;13:7801-7818. *Corresponding authors.
- Alam K, Brabant M, Solomon VR, Barreto K, Fonge H*, Geyer CR*. A novel synthetic trivalent single chain variable fragment (Tri-scFv) construction platform based on the SpyTag/SpyCatcher protein ligase system. BMC Biotechnol. 2018 Sep 10;18(1):55. *Corresponding authors.
- El-Sayed A, Bernhard W, Barreto K, Gonzalez C, Hill W, Pastushok L, Fonge H*, Geyer CR*. Evaluation of Antibody Fragment Properties for Near Infrared Fluorescent Imaging of HER3-Positive Cancer Xenografts. Theranostics. 8(17): 4856-4869. *Corresponding authors.
- Lee Y, Goyal K, Prasad B. Acute Kidney Injury in a 31-year-old Male as a Consequence of Multiple Myeloma. Cureus. 2018 Jun 26;10(6)
- Prasad B, Giebel S, Garcia F, Goyal K, Shrivastava P, Berry W. Successful Use of Renal Denervation in Patients With Loin Pain Hematuria Syndrome-The Regina Loin Pain Hematuria Syndrome Study. Kidney Int Rep. 2018 Feb 2;3(3)
2019
- Nguyen XV, Adams SJ, Hobbs S, Ganeshan D, Wasnik A. Radiologist as lifelong learner: Strategies for ongoing education. Acad Radiol. 2019 May 6. doi: 10.1016/j.acra.2019.03.019.
- Yi X, Adams SJ, Babyn P. Automatic catheter detection in pediatric X-ray images using a scale-recurrent network and synthetic data. J Digit Imaging. 2019 Apr 10. doi: 10.1007/s10278-019-00201-7.
- Baniak N, Adams S, Lee C-H, Chibbar R, Kanthan R. Extrapelvic metastases in endometrial stromal sarcomas: a clinicopathological review with immunohistochemical and molecular characterization. Int J Surg Pathol. 2019 Apr;27(2):208-215.
- Adams S, Burbridge B, Babyn P. I. Mendez. Access to ultrasound imaging: Qualitative study in northern, remote Indigenous communities in Canada. Work in Progress.
- Burbridge B, Bryce R. Venous Doppler ultrasound findings 3 months after arm port implantation thrombosis by port type within a randomized, controlled trial. Journal of the Association for Vascular Access, 2019, 24 (1): 21 – 28. https://doi.org/10.1016/j.java.2018.28.001
- Uppal J, Burbridge B, Arnason. T. Bilateral osteonecrosis of the hip in panhypopituitarism:Case Report. BMJ Case Reports, published online Feb. 22, 2019. http://dx.doi.org/10.1136/bcr-2018-227471
- Burbridge B, Burbridge C, Costa J, Carter Y. ODIN: Adaptation of an HTML 5 compatible DICOM viewer for MIRC-TFS, Enhancing the Incorporation of Clinical Images into the Health Science Curriculum. Medical Science Education, January 3, 2019 online. https://doi.org/10.1007/s40670-018-00679-w
- Hartimath SV, El-Sayed AM, Bernhard W, Makhlouf A, Hill W, Salomon VR, Parada AC, Barreto K, Geyer CR, Fonge H*. Therapeutic potential of nimotuzumab PEGylated maytansine antibody drug conjugates against EGFR positive xenograft. Oncotarget. 2019;10(10):1031-1044. *Corresponding author.
- Bernhard W, El-Sayed A, Barreto K, Gonzalez C, Fonge H*, Geyer CR*. Near infrared imaging of epidermal growth factor receptor positive xenografts in mice with domain I/II specific antibody fragments. Theranostics 2019; 9(4): 974-985. *Corresponding authors.
- Hartimath SV, Alizadeh E, Solomon VR, Chekol R, Hill W, Parada AC, Barreto K, Geyer CR, Fonge H*. Preclinical evaluation of 111In-labeled PEGylated maytansine nimotuzumab drug conjugates in EGFR-positive cancer models. J Nucl Med. 2019 Jan 17. pii: jnumed.118.220095. doi: 10.2967/ jnumed.118.220095. [Epub ahead of print]. *Corresponding authors.
- Bharathikumar VM, Barreto K, Hill W, Hogan D, Sutherland AR, Kosalik A, Fonge H, Decouteau JF, Geyer CR. Next-generation sequencing-guided and reconstruction of antibody CDR combinations from phage selection outputs. Nucleic Acids Res. 2019;47(9):e50. doi: 10.1093/nar/gkz131.
- Makhlouf A, Hadju I, Hartimath SV, Alizadeh E, Wharton K, Wasan K, Badea I, Fonge H*. 111In-labeled glycoprotein non-metastatic b (GPNMB) targeted gemini surfactant-based nanoparticles against melanoma: in vitro characterization and in vivo evaluation in melanoma mouse xenograft model. Mol Pharm. 16(2): 542-551. *Corresponding author.
- Solomon VR, Gonzalez C, Alizadeh E, Bernhard W, Hartimath SV, Barreto K, Geyer CR, Fonge H*. 99mTc(CO)3+ labeled domain I/II-specific anti-EGFR (scFv)2 antibody fragment for imaging EGFR expression. Eur J Med Chem. 157: 437-446. *Corresponding author.
- Alam MK, El-Sayed A, Barreto K, Fonge H*, Geyer CR*. Site-specific fluorescent labeling of antibodies and diabodies using spyTag/spyCatcher system for in vivo optical imaging. Mol Imaging Biol. 2019;21(1):54-66. *Corresponding authors.
- Sean K. Sethi, Shawn J. Kisch, Kiarash Ghassaban, Ali Rajput, Alex Rajput, Paul S. Babyn, Saifeng Liu, Peter Szkup, E.Mark Haacke. Iron quantification in Parkinson’s disease using an age-based threshold on susceptibility maps: The advantage of local versus entire structure iron content measurements. Magnetic Resonance Imaging 55 (2019) 145-152.
- Prasad B, Berry W, Goyal K, Dehghani P, Townsend RR. Central Blood Pressure and Pulse Wave Velocity Changes Post Renal Denervation in Patients With Stages 3 and 4 Chronic Kidney Disease: The Regina RDN Study. Can J Kidney Health Dis. 2019 Feb 13;6: 2019.
- Wolfmueller Z, Goyal K, Prasad B. Bilateral renal artery stenosis as a cause of refractory intradialytic hypertension in a patient with end stage renal disease. BMC Nephrol. 2019 Jan 14;20(1):19
| Dr. Steven Machtaler Assistant Professor |
Dr. Humphrey Fonge Radiopharmacist & Assistant Professor |
Dr. Haron Obaid Professor & Radiologist |
| Dr. David Leswick Research Director, Professor & Radiologists |
Dr. Paul Babyn Professor, Radiologist, & Physician Executive for SHA |
Dr. Farid Rashidi Program Director, Assistant Professor & Radiologist |
| Dr. Jon Tan Assistant Professor & Radiologist |
Dr. Scott Adams Departmental UGME Program Director and Radiologist |
Bruna Bonavia-Fisher College of Medicine Research Coordinator |
RUH MRI Research Team Contacts
Dr. Tasha Ellchuk
RUH MRI Section Head
306-655-2371
Jacquie Turley
Interim RUH Nuclear Medicine, PET/CT and MRI Manager
306-655-1829
Marla Komaransky
SPH Medical Imaging Manager
306-655-5144
Cheryl Sakowski
Interim SCH Medical Imaging Manager
306-655-8461
Rob German
MRI Supervisor
306-655-6656
Sharleen Maley
Research Approval Coordinator - Research Department
306-655-1442
Overview, Policies and Procedures
MRI research time will be formally offered at RUH beginning May 10, 2012 from 12:30pm to 4:00pm. This time will be reserved on every Thursday for either the 1.5T or 3T scanner (provided we have time to adjust schedule for other magnet accordingly – preferably 30 days). This time will be available for any approved MR imaging research, fMRI research, MR Proton spectroscopy research, animal research, etc. A certify MRI technologist will be available and will operate the scanner as directed and in conjunction with the researcher. Only SHR certified technologists will be allowed to operate the scanners. Onsite MRI safety for staff volunteer subjects and researchers will be the responsibility of the technologist. All human imaging subjects must read and sign a disclaimer before being imaged.
Scheduling priority(s) will be:
- Projects for which external funding is available
- Projects including SHR Imaging Department faculty
- Pilot data before REB and OA
- RUH magnet/sequence development/update time
Policies, Procedures and Communications:
- All research will need REB approval from the University of Saskatchewan research ethics board as well as operational approval from the SHR before commencement of imaging. Exceptions could be made for acquiring limited initial pilot MR image data on proposed research as approved by RUH MRI medical lead Dr. David Leswick, RUH MRI research team, or designate. Initial validation for projects pre REB and OA may be provided without formal commitment, if requested.
- All attempts will be made to schedule research time at least 3 weeks in advance.
- Initial discussion and requests from researchers should be directed to Dr. Leswick or designate. Application for research must be completed and submitted.
- Operational approval may be needed and will be granted by RUH Nuclear Medicine Manager Christine Dawson or designate.
- Communication to outside department heads regarding MRI research will be generated from the office of Dr. Sheldon Wiebe, Provinvial Head of Medical Imaging at University of Saskatchewan and Saskatchewan Health Authority.
- All researchers and assistants who will enter MRI zones III and/or IV are must complete and pass the online MRI safety program administered by SHR Quality, Safety and Informatics Manager Richard Dagenais and have site orientation done by a staff MRI technologist, supervisor, or trained MRI Radiologist.
MRI department access security prox cards will not be issued to researchers at this time as they will always be accompanied by a staff technologist or radiologist.
Process for Researchers
- Complete and submit Application for magnet research time. These forms are available in MRI department or from any research team member.
- You will be contacted for discussion/scheduling/subject safety screening.
- If approved, and you will be directly assisting with imaging, you will be directed to complete MRI safety training before beginning project.
RUH MRI Resources for Researchers
3T Siemens Skyra Tim + Dot 48 channel system with XQ gradients, 70cm bore.
- Resonant Technology Cinemavision patient video/audio LCD goggle/headset system
- Covidien Optistar Elite contrast injector
- Dedicated coils for Head/Neck 20 ch, knee 15 ch, foot/ankle 16 ch, hand/wrist 16 ch, body matrix array 18 ch, peripheral array 36 ch, posterior spine in table coil 32 ch.
- H proton MRS-single and multi, SWI, DWI, TOF MRA/MRV, Phase Contrast MRA/MRV, CEMRA/MRV, ASL, Perfusion, Cardiac Argus processing, CSF and blood flow analysis, Parallel imaging, TIM CT (continuos table movement scanning with total body matrix combined).
1.5T Siemens Avanto Tim 76 x 32 with SQ gradients, 60cm bore.
- Resonant Technology Cinemavision patient video/audio LCD goggle/headset system
- Covidien Optistar Elite contrast injector
- Dedicated coils for Head, knee, foot/ankle, wrist, body matrix array x 2, peripheral array for lower body.
- H proton MRS-single and multi, SWI, DWI, DTI, TOF MRA/MRV, Phase Contrast MRA/MRV, CEMRA/MRV, Perfusion, Cardiac Argus processing, CSF and blood flow analysis, Parallel imaging.
- fMRI protocols are currently under development, but not available at this time.
Clinical Services
 CT BOOKINGS
CT BOOKINGS
Ph. (306) 655-2399
Fax (306) 655-2387
The following CT examinations may be performed during the day or evening.
- HEAD/NECK/or CHEST CT
- CERVICAL/THORACIC or LUMBAR SPINE
- EXTREMITIES
- ABDOMEN/ABDOMEN AND PELVIS
- CT ANGIOGRAPHY
- CARDIAC/CORONARY CT
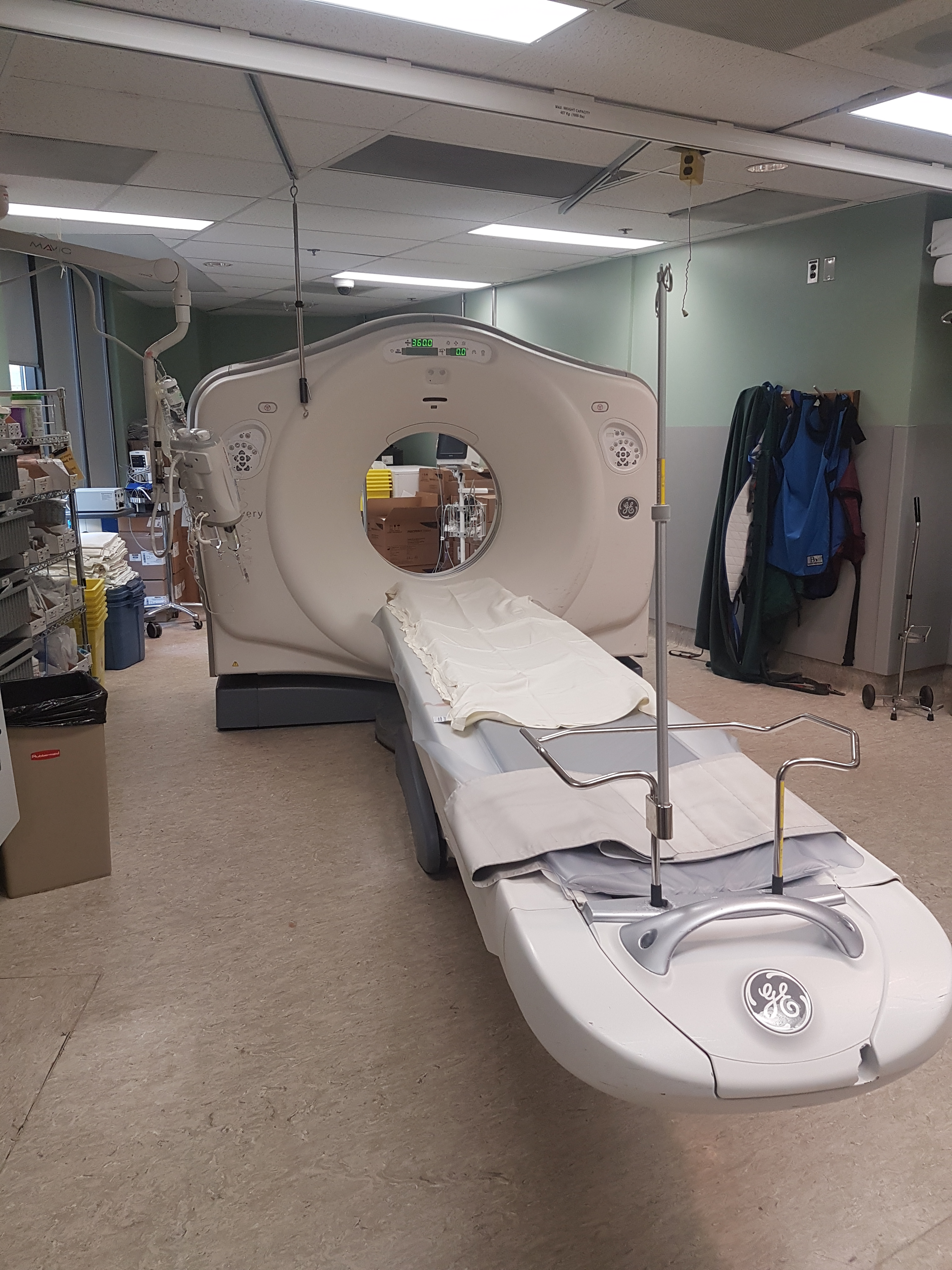
At RUH we are currently operating a GE CT750 HD Scanner and a GE LightSpeed Ultra.
RUH CT Section Head:
Derek Fladeland, MD, FRCP(C)
RUH Technologist CT Supervisor:
Lori Toews
 The General Fluoroscopy department offers many clinical services including: arthrograms, aspirations, barium enemas, modified barium swallows, small bowel enemas, cleft palates, cholangiograms, esophograms, hysterosalpingograms, GI's, myelograms, sialograms, tube checks, VCU's, venograms and fluorocopically-guided joint injections and operative procedures .
The General Fluoroscopy department offers many clinical services including: arthrograms, aspirations, barium enemas, modified barium swallows, small bowel enemas, cleft palates, cholangiograms, esophograms, hysterosalpingograms, GI's, myelograms, sialograms, tube checks, VCU's, venograms and fluorocopically-guided joint injections and operative procedures .
We are currently operating a Philips Radiography and Fluoroscopy unit and a Philips multipurpose c-arm fluoroscopy unit.
RUH General Fluoroscopy Section Head:
Ian Waddell, MD FRCP (C)
SHR RUH Technology Supervisor:
Ryan Ostrowski, RTR
An x-ray machine sends a radiation beam through the body and demonstrates solid internal structures, like bone, organs and dense muscle tissue as an image for technologists and doctors to see. Several x-rays may be taken from different angles. X-ray images are processed and ready for evaluation shortly after the procedure.Some examples of radiology tests include all bone examinations, chest and abdomen images, examinations of the stomach and bowel (barium is used to visualize the organs), examination of the kidneys by injecting a contrast (dye) into a blood vessel.
SHA Technologist SupervisorRyan Ostrowski
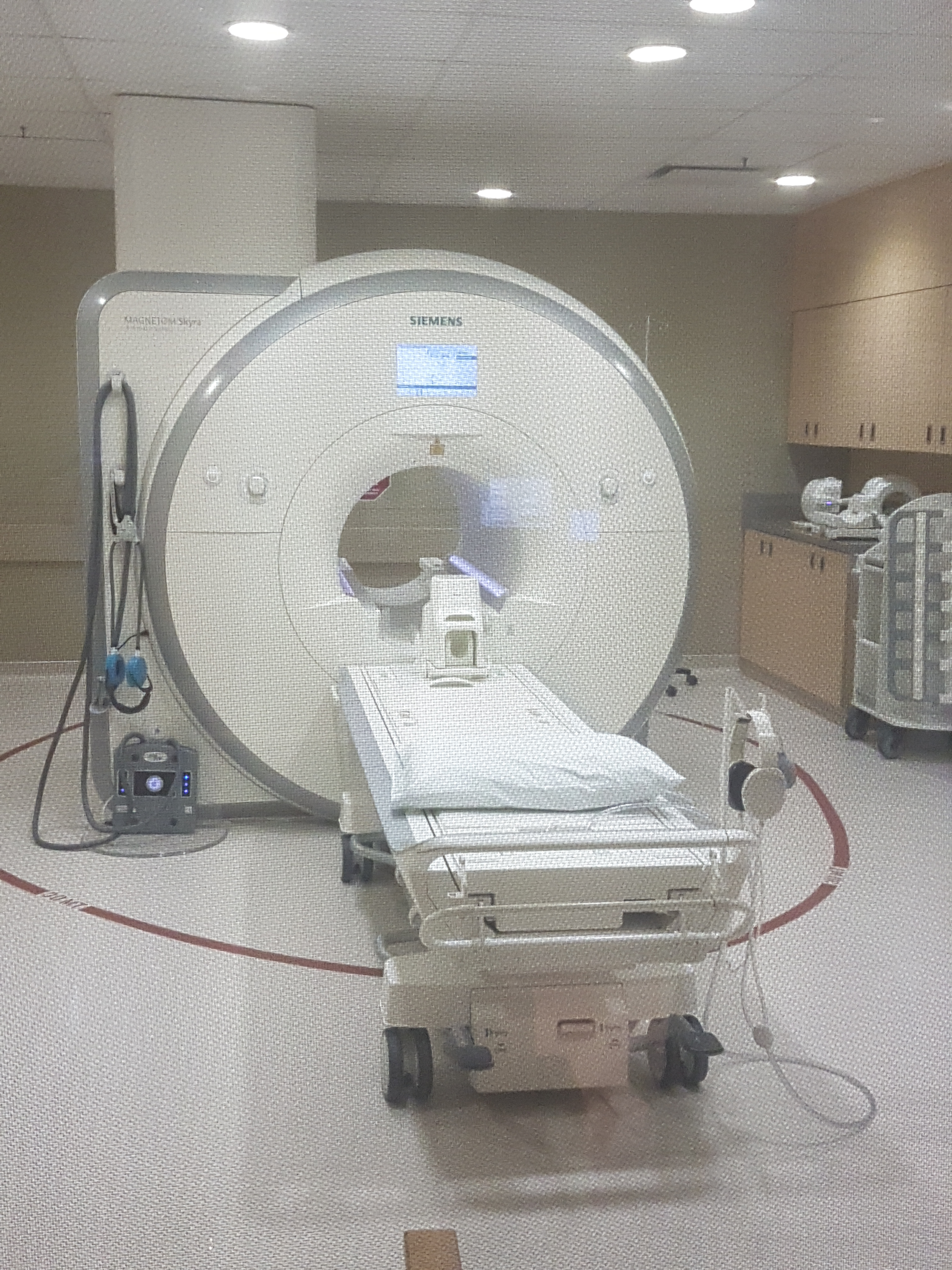 The MRI department at Royal University Hospital was opened in 1992 and continues to function as a clinical, teaching, and research magnet.
The MRI department at Royal University Hospital was opened in 1992 and continues to function as a clinical, teaching, and research magnet.
New state of art 1.5 T MRI Units were installed at St. Paul’s Hospital in 2008 andSaskatoon City Hospital in 2011.
The RUH facility currently occupies a beautiful new MR suite in the Potash Corp MRI Centre at RUH with both 1.5 and 3 T MRI Units.
The RUH MRI offers clinical diagnostic services for many departments including but not limited to neurology, neuro-surgery, general surgery, orthopedics, ophthalmology, internal medicine, cardiology, emergency medicine, and oncology. We predominantly see patients from the Saskatoon Region, and the northern half of the province, but often we receive referrals from the entire province due to our affiliation with the medical college and the many specialists who practice here. The department is involved in the specialty training of Radiology residents and MRI technologists.
We are currently operating a Siemens 1.5T and 3T MRI systems equipped and capable of doing high resolution neuro imaging, functional imaging, cardiac imaging, magnetic resonance angiography (MRA), spectroscopy, breath-hold abdominal imaging, magnetic resonance cholangio-pancreatography (MRCP), flow studies and analysis, and much more.
Requests for MRI information and/or services in this district (SPH, SCH and RUH) are currently accepted from specialists only and should be directed to MRI Central Booking office:
Ph: (306) 655-2412Fax: (306) 655-2416RUH MRI Section Head:
David Leswick, MD, FRCP(C)
RUH Technologist Supervisor:
Robert German
Nuclear Medicine is a discipline of Diagnostic Imaging that focuses on the physiology of the body or the functional cells. We have tracers that are made radioactive and then they are injected usually intravenously into the body enabling us to image specific cells in the body as they are functioning.
Images are much longer than an “xray” as we are actually imaging the function of those cells. Testing times vary from 30 minutes to multiple day images.
The radiotracers are safe and patients will experience very little or no side effects from these radiotracers.
Common studies performed :
Myocardial Perfusion ImagingBone Scans
Lung Scans
Thyroid Studies
Gastric Emptying Studies
Parathyroid Studies
Bone Mineral Densitometry
Therapeutic Services
HyperthyroidismThyroid Ablation
Radium Prostate Metastatic Therapy
Physician Information
We operate departments at:
- RUH -3 GE Hawkeye cameras and, a GE Discovery 530 cardiac camera,
- SPH -1 GE Hawkeye and a shared hybrid unit a Siemens Symbia Intevo 16 SPECT/CT unit that is shared with the CT department
- SCH has a GE Hawkeye and 2 Hologic Bone Mineral Densitometry units.
ALL bookings are coordinated from the RUH booking office and all requisitions must be faxed to 306-655-1742, Appropriate requisitions must be completed and faxed to the department before any study will be scheduled.
There are 3 requisitions to choose from :
Clinical Services are available 0800-1630 Monday-Friday and On call services are available at RUH weekends and stat holidays 0900-1700. The department can be contacted through Switchboard for on call service Questions and concerns may be directed to :
Department of Nuclear Medicine
Royal University Hospital
103 Hospital Dr.
Saskatoon, SK. S7N 0W8
Phone: (306) 655-1797
Fax: (306) 655-1742
Dr Sundeep Nijjar
Department Head Nuclear Medicine
Saskatchewan Health Authority
Office: (306) 655-1797
Physician Contact
Saskatchewan Health Authority
Office: (306) 655-2932
Christine Dawson
RUH Manager of Nuclear Medicine and PET/CT Services
Phone: 306-655-1829
Shane Timm, RTR
RUH Director of Medical Imaging
Saskatchewan Health Authority
Office: (306) 655-1802
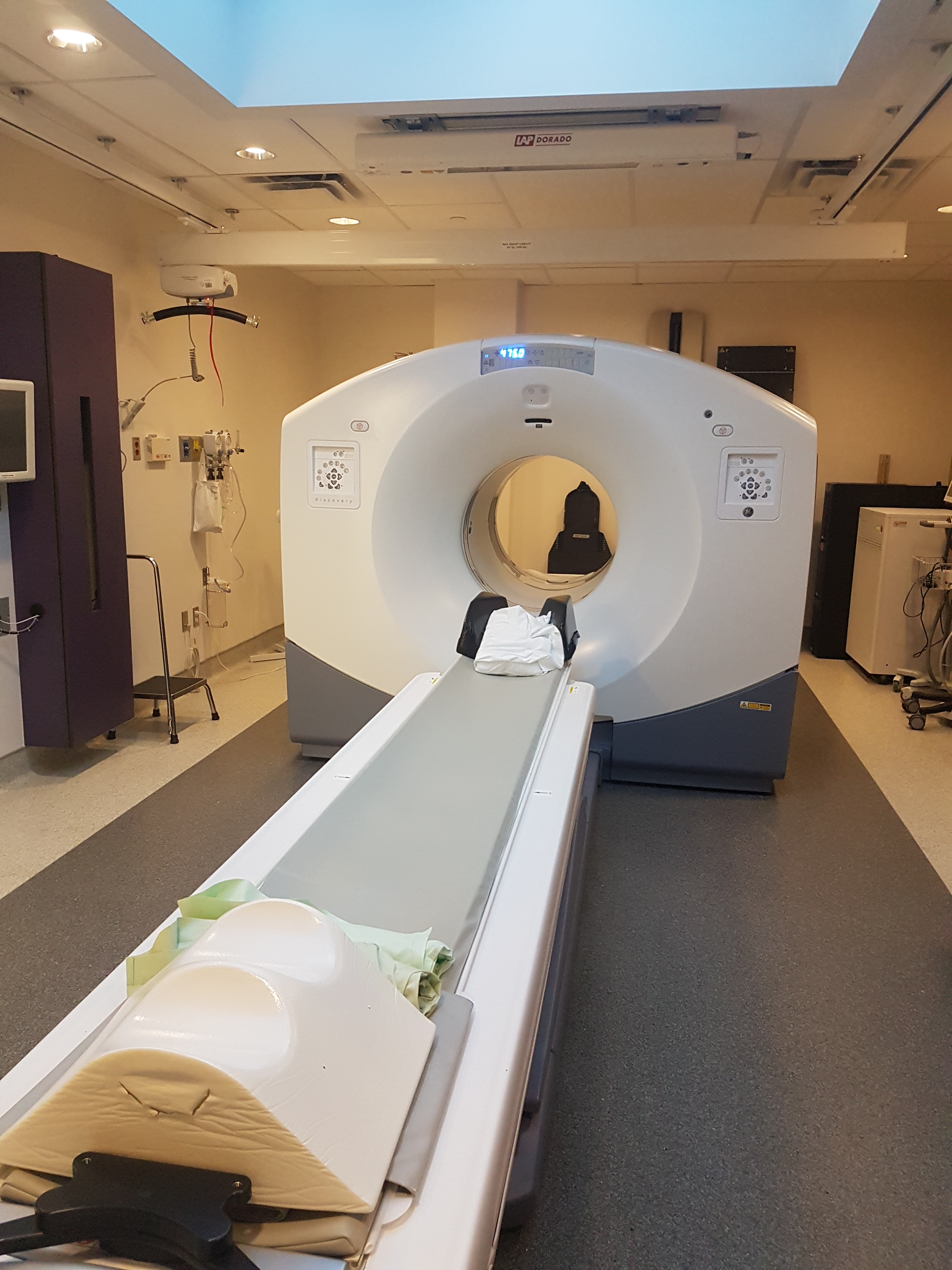 Positron Emission Tomography-Computed Tomography (better known as PET/CT) is a diagnostic technique that incorporates both a PET camera and a CT scanner into one imaging device. Through this process clinicians are able to incorporate the strengths of a PET camera by looking at the body's cells at a molecular level while adding the anatomic accuracy of a CT scanner to pinpoint where disease processes are occurring.
Positron Emission Tomography-Computed Tomography (better known as PET/CT) is a diagnostic technique that incorporates both a PET camera and a CT scanner into one imaging device. Through this process clinicians are able to incorporate the strengths of a PET camera by looking at the body's cells at a molecular level while adding the anatomic accuracy of a CT scanner to pinpoint where disease processes are occurring.
In essence, two exams are performed sequentially and the images from both modalities are fused together to give the interpreting physician a more comprehensive picture from both a molecular and an anatomical standpoint. When PET and CT images are combined, physicians can view the exact location and extent of disease, allowing for an accurate diagnosis and precise roadmap to guide treatment.
For Patients:
What is PET/CT?
PET stands for: Positron Emission Tomography The test begins with an intravenous injection of a radioactive sugar called FDG (fluorodeoxyglucose). The sugar shows up in areas of your body where the cells are more active or have a higher "metabolic activity" than normal.
CT stands for Computed Tomography (a 3-D x-ray imaging technique). CT helps to localize the FDG uptake to specific anatomic structures. An abnormality detected by CT will be shown to represent active disease if the metabolic activity is high on the PET scan. Many normal cells like muscle and white blood cells also use sugar as fuel. CT will help to localize the FDG activity to normal or inflamed arthritic joints and avoid a misdiagnosis.
What to Expect
What can I expect once I arrive?
When you arrive, a technologist will review your information and answer any additional questions you may have. You will need to fast for several hours prior to the examination so that the cells in your body are able to take up the FDG (radiotracer). You should only drink plain water up until your appointment time to avoid dehydration.
Initially your finger will be pricked and your blood sugar will be measured using a glucometer to ensure that your blood sugar is within acceptable limits for your examination. You will be weighed and an IV will be started in your hand or arm. You will then be placed in a warm dimly lit room and made as comfortable as possible. Next, a small amount of the radiotracer will be injected into the IV. The IV will be left in for the duration of the scan.
You will NOT be able to listen to music, read, talk, or play video games, etc. It is important that you remain in a resting state and are stimulated as little as possible in order for the FDG (radiotracer) to be fully effective. You will remain in a room resting for approximately 45 minutes to an hour prior to your scan. When it is time for your scan, the technologist will ask you to empty your bladder just before your scan begins.
What will the scan be like?
You will lie on a comfortable table that moves slowly through a ring-like scanner as it takes the pictures. You may be asked to raise your arms or place them on your abdomen depending on what type of study you are having. It is important that you lie very still during your exam because movement can interfere with obtaining proper results. The first part of the procedure is a CT scan which will take about 30 seconds. The PET scan takes on average an additional 30-45 minutes. Both procedures are performed on the same machine. Once your images have been checked to ensure that all information is of diagnostic quality, you will be free to leave.
How long does the procedure take?
Plan to spend about 2 hours with us, from the moment you arrive until you are ready to leave. This time will vary slightly depending on the type of examination you are having.
What happens after the exam?
You may leave as soon as the exam is completed. If you received a sedative prior to the exam, you must have a pre-arranged ride home. You will be able to eat and drink immediately after the exam. Drinking fluids is encouraged to remove any FDG from your system. The nuclear medicine (PET) specialists will review the images from your PET/CT and send a report to your referring doctor.
Contact your doctor for your results of the PET/CT.
Who should I contact if I have questions?
If you have questions about a PET/CT that has already been booked call (306)-655-3340. If you have any other questions contact your physician.
What are the risks associated with FDG PET/CT?
The amount of radiation you receive from a PET scan is comparable to any other radiography procedure such as a CT or Bone Scan. You will be slightly radioactive for several hours so you should stay 5-6 feet away from an infant, or anyone who is pregnant after you leave. You may interact freely with other adults. FDG will no longer be detectable in your body after 24 hours.
If you are pregnant or breast feeding you should inform the imaging staff BEFORE the examination is performed.
For Pediatric Patients
How long does the procedure take?
You can expect to be in the PET/CT department for approximately 2-3 hours. It's important you arrive 30 minutes before your child's appointment. When you arrive your child will be checked in to the department, then a technologist will interview you and your child to ensure that all the conditions have been met to proceed. An intravenous will be set up and then some radioactive material called FDG will be injected and allowed to work in the body for about an hour. The actual scanning portion of a PET/CT exam takes approximately 30-45 minutes.
What if my child won't hold still for the 45 minute scan time?
If a child is under the age of 5 or you know they will not be able to hold still for the scan we may need to arrange sedation for your child. This is something you can talk to your physician about or you may contact us at (306) 655-3340 and we advise you on a course of action.
Is it dangerous for my child to get this scan?
The radioactive material FDG has been proven to have no side effects to a patient. It works just like glucose or sugar in your body; which is why we must wait an hour before scanning so we allow the body to naturally process this material the way it would with other sugars. There is some radioactivity involved but pediatric patients receive much less of a dose than adult patients. There is a CT component to the scan but unless indicated that it is a full CT with contrast it is less radiation than a normal CT scan. The Saskatoon Health Region works hard at implementing ALARA (As Low As Reasonably Achievable), which means we want to give as little radiation as possible to still get pictures of diagnostic quality. If you have any questions you may phone our Radiation Safety Officer for further clarification at (306) 655-1797
What preparation does my child need to do before coming?
- Your child needs to be fasting the morning of the scan. This means no food or drink is allowed but they may have as much water as they want. Things such as gum and cough syrup are not allowed as well.
- Strenuous activity should be avoided for 24 hours before the scan.
- Being cold right before coming to the scan can interfere in obtaining proper results so if it is winter pre heating your car before coming and wearing warm clothing can make the images turn out better.
- Dress the child in comfortable clothing avoiding metal snaps or zippers. This can interfere in obtaining proper results. After arrival we may need them to change into a hospital gown.
- If your child is diabetic please contact us as we may need to issue special instructions.
- The day before the study it is important to have a low carbohydrate, low sugar diet. This means things like potatoes, rice and candy should be avoided. Things high in protein like meats and cheeses are good to eat.
Can I stay with my child for the scan?
You should be able to be with your child almost the whole time they are in our department. The only time you may be asked to leave is when the CT scanner is going but this takes only about a minute and you would be able to return to your child’s side after this.
How do I let my child know what is happening before the test?
Before the test talk to your child about what they can expect. For young children, use simple words and explain only shortly before the test is scheduled to start. Some children are most afraid that we need to give them a needle so you may want to avoid telling them that before they come. This is dependant on your child, you know them best.
Patient Preparation Instructions
Please refer to Patient Information & Instructions for PET/CT Examination to obtain diet instructions prior to your PET/CT examination.
Physcian Information
Clinical PET/CT Services
The PET/CT department at the Royal University Hospital is equipped with a Discovery 710 PET/CT scanner from G.E. Medical Systems, the first of its kind to be released in Canada. The new facility has the ability to provide PET scans with diagnostic contrast enhanced CT, as well as PET/CT with radiotherapy planning.
There is also the opportunity to provide certain types of cardiac, and neurological imaging as well.
Referrals
Referrals are accepted according to clinical indications set forth by the medical requisition located in the link below.
Clinical services are offered Monday to Friday. PET/CT requests are only accepted from approved specialists at this time. Questions or concerns can be directed to:
PotashCorp. PET/CT Department
Royal University Hospital
G606, 103 Hospital Dr.
Saskatoon, SK. S7N 0W8
Phone: (306) 655-3340
Fax: (306) 655-1635
Dr. Abdulaziz Almgrahi MD, FRCPC, ABNM, CBNC
Clinical Head of PET/CT Operations
Saskatchewan Health Authority
Office: (306) 655-1797
Christine Dawson
RUH Manager of Nuclear Medicine and PET/CT Services
Phone: 306-655-1829
Shane Timm, RTR
RUH Director of Medical Imaging
Saskatchewan Health Authority
Office: (306) 655-1802
Scott Mildenberger, RTNM
PET/CT Supervisor
Saskatchewan Health Authority
Office: (306) 655-3357
Clinical Indications
Adult Clinical Indications
Pediatric Clinical Indications
 Ultrasound is a complex, versatile and non-invasive medical imaging tool. It is the detection and display of acoustic energy reflected from soft tissue interfaces within the body. These reflections provide the information needed to form high resolution gray scale images of the body and the study of blood flow.
Ultrasound is a complex, versatile and non-invasive medical imaging tool. It is the detection and display of acoustic energy reflected from soft tissue interfaces within the body. These reflections provide the information needed to form high resolution gray scale images of the body and the study of blood flow.
This images are obtain by highly trained credentialed sonographers using a combination of skills such as; knowledge of the physical principles of ultrasound and good understanding of pathology, physiology and anatomy.
The Ultrasound Department offers diagnostic services to many departments such as: medicine, surgery, obstetrics and gynecology, pediatrics, outpatients, emergency, neurology and nephrology
The examinations offered by the ultrasound department include; abdominal and small parts, muculoskeletal, obstetrics and gynecological, vascular, urological, trans-cranial Doppler and pediatrics.
There are five state of the art ultrasound units in the department at Royal University Hospital, three Philips IU22; one Spencer Technology for trans-cranial Doppler studies and one Zonare portable unit.
RUH Ultrasound Section Head:
Dr/ Tina Theoret, MD, FRCP(C)
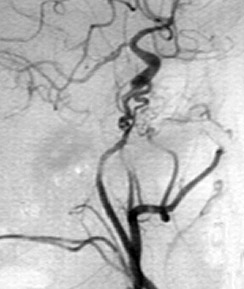 The Vascular / Interventional Radiology department offers many clinical services including:
The Vascular / Interventional Radiology department offers many clinical services including:
- Cerebral Angiography
- Other Angiography
- Venography
- Venous Access Devices
- Ovarian Vein Venography and Embolization
- Fallopian Tube Catheterization
- Fine Needle Biopsy of the Lung
- Fine Needle Biopsy - Solid Organ, Thyroid and Superficial Masses
- Core Biopsy - Liver, Thyroid and Superficial Masses
- Drainage Tube Checks and Changes
- Gastrojejunostomy
- Neuroradiology Interventional procedures
- Tomuor Embolization/Ablation
- Varicocoele Embolization
- Uterine Artery Embolization
At RUH we are currently operating a Philips, Allura Xper, bi-plane, digital detector, fluoroscopy unit.
RUH Vascular / Interventional Radiology Section Head:
Dr. Peter Szkup, MD, FRCP(C), FCR(D)SA, MMed(UCT)
Other Radiologists active in the RUH section:
Dr. Brent Burbridge, MD, FRCP(C)
Dr. Rob Otani, MD, FRCP(C), BSc
Dr. Grant Stoneham, MD, FRCP(C)
RUH Technologist Manager:
Darin Humphreys
RUH Vascular Supervisor
Brian Heck
Medical Image Solution for Teaching and Research
What is MISTR?
Medical Image Solution for Teaching and Research. The solution in its current incarnation, in broad strokes, is an online electronic systems that would include the following capabilities: provide faculty with electronic capability to develop teaching case files based on DICOM images from local radiology equipment. Provide students with the capability to study cases and train and provide summative assessment of learning. Provide researchers with the capacity to pull DICOM images and data from existing repositories and equipment to develop a database of clinical cases for research purposes.
Characteristics of the system:
- Capability to display DICOM (w/full control) and non-DICOM images.
- Include the ability to store meta-data, case history and other medical information that aid in differential diagnosis.
- Must be accessible via a secure connection through the web (HTTP) or (HTTPS).
- Must preserve all DICOM capabilities.
- Anonymize patient information to protect confidentiality.
- Closely mimic clinical systems in look and feel and capability.
- Roles include faculty, student, researcher
The purpose of this wiki is to provide instructions and help for the MISTR Tool suite.
News
Loading...
Events Calendar
Loading...
Contact
Department of Medical Imaging
Saskatchewan Health Authority and University of Saskatchewan
103 Hospital Drive, Room 1566
Saskatoon SK
S7N 0W8
Erin Cook
Executive Assistant to the Provincial Head, Department of Medical Imaging Dr. Sheldon Wiebe
Phone: 306-655-2402
Fax: 306-655-2370
Requisitions & Referrals Fax: 306-655-6784
Amanda O'Leary
Senior Residency Program Administrator
Fluoro and Vascular patient inquiries, please phone: 306-655-2374
CT and Ultrasound patient inquiries, please phone: 306-655-2399
General X-ray patient inquiries, please phone: 306-655-2371
MRI patient inquiries, please phone: 306-655-2412
NM patient inquiries, please phone: 306-655-1797
PET/CT patient inquiries, please phone: 306-655-3340
